Three-dimensional imaging is no longer just a gimmick for producing interesting fetal "keepsake" pictures to show expecting parents. The rise of 3D imaging is now being driven by necessity rather than novelty, and is leading to a revolution in the way radiologists think about the data they manipulate and review.
Multislice CT scanners produce more 2D slices than anyone has time to read, or even display on a lightbox, so radiologists are turning to 3D to not only cope with masses of data but also to convert stacked 2D slices into 3D volumes.
And 3D ultrasound has virtually revolutionized ob/gyn and cardiology.
"(Three-dimensional) imaging has the ability to display in a single image or a fewer number of images the same amount of information that require hundreds or even thousands of 2D axial images to see the same information," said Tom Naypauer, product manager of CT visualization for Philips Medical Systems of Andover, MA.
The problem of mountains of data is being addressed by the Society of Computer Applications in Radiology (SCAR) through its Transforming the Radiological Interpretation Process (TRIP), an interdisciplinary initiative to focus research and discovery of solutions to information and image data overload.
The SCAR TRIP initiative focuses on improving efficiency of interpretation of large datasets, improving the timeliness and effectiveness of communication, and decreasing medical errors.
Imaging used to be exclusively 2D. But everything about human organs is 3D; 2D imaging was used for want of 3D imaging capability.
For instance, radiologists doing a two-view chest study use their imagination to create a mental 3D reconstruction, going back and forth between the views. Some studies required more than two views to provide enough information for the radiologist, the orthopedic surgeon, and the cardiologist to create a mental picture.
Cross-sectional CT and MRI studies, along with the development of ultrasound, changed all that. What was once thought to be a gimmick is now about to become the standard of care. With volume imaging, the data exists to make 2D sections of a 3D whole.
Surgeons operating on a tumor don't cut out a 2D slice, so why not look at a 3D image? A 3D image can tell the surgeon what he or she will find in the OR. And since noninvasive exams, or minimally invasive procedures such as catheter-based scans, are generally better for the patient than general anesthesia and surgery, using 3D images of the target site will allow more and more procedures to be done percutaneously.
 |
| CTA, volume-rendered view of aortic dissection. Image courtesy of TeraRecon. |
  |
CTA, volume-rendered view of aortic dissection. Clip courtesy of TeraRecon. |
Chest radiographs are increasingly being used primarily to see where life-support lines have been placed, or for imaging pneumonias. For lung cancer, the number of false-negatives with traditional x-ray is so great that anyone suspected of the disease is almost automatically scanned with CT. Studies at the University of Maryland with CT radiation dose levels almost as low as traditional chest x-ray are showing a significant level of accuracy, and with an increase in patient throughput, CT may replace standard radiography for chest screening.
Integration of 3D with PACS is still in its infancy, but will be a key component of the next phase of product development. Present-day efficacy varies widely from one vendor to another. A convergence for all the modalities along with 3D is evolving, so that radiologists will be able to call up software for whatever studies they are reading, and read what looks like an image from the PACS network.
Applications
Given that our bodies come off the shelf in 3D, the uses of 3D imaging seem limitless. Dr. Christoph Wald, director of the 3D lab at the Lahey Clinic in Burlington, MA, believes any type of advanced quantitative imaging is a prime candidate for using 3D. And this is just the tip of the iceberg.
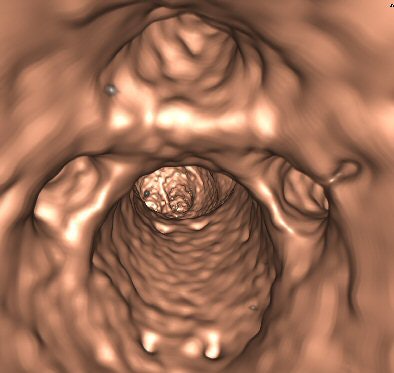
Uses can include calculation of complete or partial organ volumes (such as in live donor liver transplant planning), tumor volume measurement, and lung nodule analysis; operative planning, such as partial nephrectomy or other complex solid organ surgery; planning for interventional procedures such as 3D CT cholangiography prior to percutaneous biliary procedures; abdominal aortic stent graft planning in which measurements are taken to build a custom-made graft; any type of CT angiography (CTA) or MR angiography (MRA), like of the head and neck, periphery, and abdomen; epilepsy surgery planning; and virtual colonoscopy, virtual bronchoscopy, or cardiac imaging (functional and coronary).
 |
| The ability to visualize simultaneously in the axial, coronal, and sagittal planes and to perform a 3D fly-through of the colon can improve efficiency and accuracy in the detection of polyps and other pathology for virtual colonoscopy. Image courtesy of Dr. Eliot Siegel. |
  |
A multiplanar 3D workstation can provide real-time interactive navigation and visualization of the abdomen and chest in the coronal and sagittal in addition to the axial planes. Clip courtesy of Dr. Eliot Siegel. |
  |
3D colon fly-through from a CT scan. Arrow marks potentially cancerous polyp. Clip courtesy of Vital Images. |
  |
MRI-based 3D image of a patient with a meningioma, demonstrating its relationship to the brain surface for neurosurgical resection planning. Clip courtesy of Dr. Christoph Wald and Dr. Horst Hahn, MeVis, Bremen, Germany. |
Yet to integrate 3D review into the diagnostic reading process efficiently, one needs a bevy of personal skills, combined with ready access to a workstation, a tightly integrated PACS/3D solution, or trained technologists who preprocess the images, Wald said.
And he cautioned that because most processing involves manual cutting, automatic segmentation, or threshold-based segmentation (i.e., the removal of information to enhance what one is clinically interested in), there is ample opportunity to remove vital information or even to create "pseudolesions." Therefore, the radiologist needs to be familiar with the pitfalls and recognize them.
"It's hard to see what's not there," Wald said.
Many radiologists use 3D in specialized applications. Dr. Joel Neuman, director of cardiovascular imaging at Zoom Imaging in Lehigh Valley, PA, applies the technology to vascular imaging.
"It provides a rapid overview of potential areas of pathology when dealing with large volume datasets (e.g., peripheral CTA) by quickly identifying areas of noncalcified stenoses and easily identifying calcified plaque, which can then be interrogated further with other tools," Neuman said. "I am using (volume rendering) mostly in the workup of primary vascular disorders or in problems solving cases where there is vascular involvement secondary to another disease process (tumor, inflammation, etc.)."
 |
| Endoscopic view of abdominal aortic aneurysm. Image courtesy of Barco. |
  |
3D color volume reconstruction of an abdominal aortic aneurysm. Clip courtesy of Dr. Paul Curtis of South Jersey Radiology Associates, and Barco. |
Ob/gyn
Fetal facial images in 3D ultrasound attracted mass media attention a few years ago. Although it gave facial pictures of fetuses that could be shown to parents before their babies were born, ultrasound could also show cleft lips and other deformities, so pediatricians would know what procedures might have to be performed right after birth. Now, going one step further, it can indicate whether the procedure can be done intrauterine before birth.
It is difficult to downplay the impact of 3D ultrasound on obstetrical practice.
"(Three-dimensional) ultrasound provides more accurate diagnoses for a variety of obstetrical and gynecological conditions, helping physicians make diagnoses that are difficult or impossible using 2D imaging," said longtime obstetrical ultrasound researcher Dr. Dolores Pretorius of the University of California, San Diego. "(Three-dimensional) ultrasound is valuable in diagnosing and managing a variety of uterine abnormalities."
Compared with MRI, 3D ultrasound has the same capabilities but is faster and less expensive, Pretorius said. In infertile patients, or those who have had repeated spontaneous abortions, 3D is superior in identifying the specific cause, such as whether a patient has a septate uterus that requires surgery to allow gestation, or a bicornuate uterus, which requires major surgery.
Three-dimensional ultrasound does such a good job of identifying these conditions, Pretorius said, because the entire uterine volume can be acquired, and coronal images of the uterus can be viewed in a standard orientation -- something not possible with 2D ultrasound. The endometrium and myometrium can be imaged in the same plane.
If an ob/gyn physician wants to examine thickened endometrium using sonohysterography to identify the location and number of polyps, abnormal bleeding, or adhesions, 3D allows a coronal view for better visualization of the uterine anatomy.
Three-dimensional sonohysterography takes just seconds, because images are acquired rapidly from one volume acquisition, Pretorius said, adding that the coronal view captured by 3D ultrasound provides a better image of cornual and cervical ectopic pregnancies, which are difficult to assess using 2D ultrasound.
Moreover, 3D ultrasound is faster and more comfortable for the patient than 2D, because saline injected into the uterus to distend the endometrium must remain there for a shorter period, she said.
"Beyond 'pretty faces,' 3D plays a valuable role in assessing fetal anatomy to diagnose a variety of fetal abnormalities, such as malformations of the face, brain, limbs, and skeletal structures," Pretorius said. "3D ultrasound reveals facial abnormalities, such as cleft lip and palate, micrognathia, or other abnormal profiles that can be overlooked by 2D ultrasound in the clinical setting."
Cardiology
In modern hospitals, almost every cardiac patient gets echocardiography, sometimes daily, because the cost of ultrasound machines is relatively inexpensive compared to CT or MR.
Cardiologist Dr. Natesa Pandian, director of the echo lab at Tufts-New England Medical Center in Boston, calls ultrasound/echo one of "the most democratic diagnostic tools in the world, because rich or poor, everyone has ultrasound, while not everybody can afford MR or CT."
 |
| Three-dimensional method of quantifying LV volumes, ejection fraction from a real-time 3D echocardiography study. Image courtesy of Dr. Natesa Pandian. |
  |
Long-axis view of a live 3D echocardiography image from a patient with hypertrophic obstructive cardiomyopathy, showing septal hypertrophy and systolic motion of the mitral valve. Clip courtesy of Dr. Natesa Pandian. |
  |
Volume-rendered image of the heart. Image courtesy of Philips Medical Systems. |
CT is an alternative for studies such as echocardiography and nuclear medicine that have traditionally been performed by cardiologists. Similar information can be done using CT or MR in a single scan, according to Dr. Eliot Siegel, chairman of radiology at the University of Maryland School of Medicine in Baltimore.
"These are becoming routine applications for computer workstations," he said.
Reimbursement
Reimbursement will likely have an effect on the turf wars between radiologists and cardiologists, Siegel believes.
"It will come in the form of modifications in the reimbursement model, where for example, hospitals will just get one fee as patients come in, as in the DRG (diagnosis-related-group) scheme, for taking care of that patient, so the incentives to do multiple overlapping, repetitive workups will decrease," Siegel said.
But radiologists are too expensive to be doing routine 3D processing and segmentation work, Wald said.
"This should be done by trained techs or trainees under close supervision of experienced staff physicians who are able to recognize pitfalls, errors in processing, etc.," he said. "The mandatory 3D processing associated with CTA and MRA requires additional staff in any practice that does a significant number of these types of cases. Software available on scanner consoles is suitable only for performance of the most basic 3D processing (multiplanar views). For all the more advanced processing, a 3D workstation is necessary, which means additional cost for hardware and service/future upgrades," Wald said.
 |
| Volume-rendered 3D CT angiogram shows head with intracranial vessels. Large basilar tip aneurysm is marked with an arrow. Image courtesy of Dr. Christoph Wald. |
  |
CT angiography volume-rendered image showing arterial circulation of the head and neck. Clip courtesy of GE Healthcare. |
Current reimbursement doesn't reflect this increased cost of doing business, however. CTA examinations are becoming very common and are replacing in many instances more invasive, dangerous, and expensive catheter-based angiography procedures. Therefore, the level of reimbursement should adequately reflect the effort and cost associated with performance of these studies.
"Payors need to recognize the fact that 3D imaging, especially when associated with these types of exams, is good patient care and saves money by replacing some of the older techniques," Wald said. "This shift in the paradigm of how patients are studied needs to be reflected in the reimbursement."
There is some Medicare coverage for 3D imaging now. It used to all be covered, but now vascular is separated out. Reimbursement for 3D is incorporated into the exam. As a result, radiologists do not get paid a supplementary fee for doing 3D work involved with CTA and MRA.
"Basically, there is a methodological problem with the Hospital Outpatient Prospective Payment System (HOPPS) for new procedures in terms of how they are charged and how they are calculated for reimbursement," said Gordon Harris, Ph.D., director of the 3D lab at Massachusetts General Hospital in Boston. It's a process that "will penalize most new procedures such as CTA."
New procedures are either underfunded, or hospitals have to increase their charges by several multiples to be reimbursed as they should for those procedures, he said. An expert Medicare advisory panel makes recommendations to the Centers for Medicare and Medicaid Services (CMS), but Medicare is unlikely to make significant changes upward in 3D reimbursement without intervention by the U.S. Congress, Harris said.
Beyond the urban medical center
And what about the smaller community hospital that is often left out of the latest medical advances? Nestled in the heart of North Carolina's Blue Ridge Mountains is Hendersonville, county seat of 80,000-population Henderson County.
A 10-radiologist group covers three area hospitals -- the smallest 50 beds, the largest 230. Margaret R. Pardee Memorial Hospital, the largest facility, has a PACS network from Fujifilm Medical Systems of Stamford, CT, and two AW4.2 digital workstations by GE Healthcare of Chalfont St. Giles, U.K.
Dr. Bob Klym is the lead 3D practitioner at Margaret Pardee. Klym and his colleagues use two GE MR scanners and two CT machines, one four-slice and the other 16, but do 3D volumes on CT only. Klym says he gets good volume reconstruction for both CT scanners, using the four-slice mostly for bone and the 16-slice for vascular studies such as for aortic aneurysms and carotid arteries.
"We also use 3D for lung nodules, because it measures more accurately, where the radiologist might get different measurements each time," Klym said.
 |
| Three-dimensional lung segmentation of a CT image. Image courtesy of Vital Images. |
Klym said the drawbacks are radiologists who won't do 3D, and technologists who initially resisted training in the technology. And ultrasound studies can go on their PACS, but only in designated planes, not entire dynamic studies.
During some weeks, Klym's facility performs as many as 10 CTAs, then has weeks without performing any. Most orthopedic surgeons like 3D for surgical planning, which the hospital has provided since they began using the four-detector scanner five years ago, he said.
"It probably gets us a little extra business because they know we're going to do 3D, but it's not huge," Klym said. "We have this podiatrist who always wants the 3D so he can show patients what he is going to do. I think that actually gets us more cases, but it's not dramatic."
Klym believes that as radiologists accept the value of 3D imaging, smaller hospitals will eventually be forced to adopt 3D and PACS.
"It may become a standard-of-care issue," he said. "Sooner or later it's a trickle-down effect. Every town eventually gets a McDonald's."
The future of 3D imaging
Different specialties use 3D to different degrees. Neurosurgeons and orthopedic surgeons are rapidly adopting 3D for surgical planning. 3D makes images much more intuitive to them, allowing for visualizing a target in multiple planes before operating or in radiation therapy planning. And it makes more sense when trying to explain procedures to patients.
PET/CT devices are now selling in greater quantities than PET devices alone, according to Carter Yates, senior director of marketing for the Voxar product group of Barco in Kortrijk, Belgium. This trend makes visualization and analysis of fused PET/CT images an important application for volume rendering.
In the next few years, 3D workstations will be a common sight not only in radiology departments, but throughout hospitals and in physicians' offices. The funneling of these 3D images to referring physicians remains a critical obstacle, however, complicated by the varying levels of Internet connectivity at physicians' offices.
But, ultimately, physicians without 3D capability are fast becoming an anomaly.
"The big shift has been from film to filmless," Siegel said, "and now we're seeing a major shift in thinking of patients as volumes, rather than as just a bunch of axial slices."
By Robert Bruce
AuntMinnie.com contributing writer
May 2, 2005
Related Reading
VC study finds thin slices more important than low noise, April 27, 2005
4D ultrasound shows promise for improving fetal echocardiography, April 6, 2005
3D volume US shows promise for second-trimester fetal evaluation, March 17, 2005
3D ultrasound poised to revolutionize pelvic imaging, September 9, 2004
3D and the future of imaging, November 3, 2003
Copyright © 2005 AuntMinnie.com