Tumor assessment criteria that account for both tumor density and volume more accurately reflect tumor burden, and they may improve treatment monitoring by predicting outcomes earlier than methods that rely only on tumor density, according to research from the U.S. National Institutes of Health (NIH).
In a study presented at the American Society of Clinical Oncology (ASCO) annual meeting earlier this month, Dr. Les Folio showed how its combined density and volume assessment criteria -- called Automated Density and Volume Application (ADaVA) -- outperformed the Response Evaluation Criteria in Solid Tumors (RECIST) and other criteria for predicting survival in metastatic bladder cancer patients.
"Although this is a small sample of patients in an ongoing trial at the NIH Clinical Center, criteria that consider volumetric density such as ADaVA appear to correlate better with important outcomes and at earlier time points -- as early as the first follow-up exam," Folio told AuntMinnie.com. "ADaVA overall density-volume analysis was best able to predict overall survival from the first follow-up CT for metastatic urothelial cancer patients."
Density plus volume
Oncologists and radiologists agree that current imaging assessment of tumor response to treatment should take into account tumor density and volume, especially in patients on antiangiogenic therapy. After oncologists asked the NIH team a few years ago to look into quantifying densities and volumetric sizes, the group began testing this concept on the U.S. Food and Drug Administration (FDA) lung phantom, Folio said.
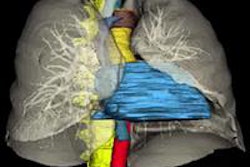
It's now accepted that 2D axial-only measurements do not accurately represent 3D tumors, Folio said. As demonstrated on their PACS (Carestream Health), current PACS tools can directly measure tumor volumes, which is an inherently more valid approach, he said.
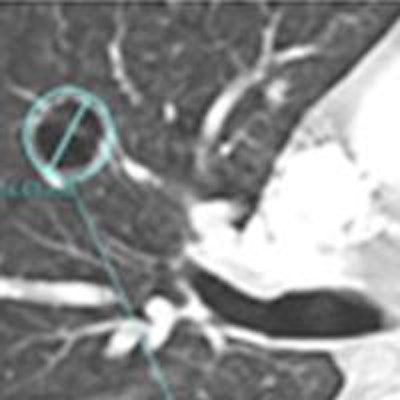
Folio noted that a decrease in tumor density due to necrosis shown on contrast-enhanced CT can be paired with an increase in axial size despite a qualitative response to targeted treatment. Metastatic lesions often show peripheral enhancement along with nonenhancing central components, he said.
"For example, lung lesions may cavitate and measure larger on axial slices, despite showing less volume of tissue, with live tumor remaining only in the peripheral rim," he said. "The manifestation of response is reflected in decreased density [that] is incompletely captured in RECIST, which gives us the opportunity to develop more appropriate criteria and tools for this general type of therapeutic response."
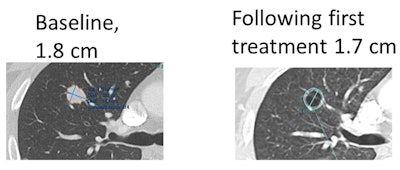 Example of metastatic lung lesion that became cavitary on the first CT following initiation of treatment. Most of the lung lesions in this patient became necrotic to the point of cavitation (commonly seen in this treatment) following the start of therapy. The lesions stayed the same size, however, and some measured larger on axial dimension. All images courtesy of Dr. Les Folio.
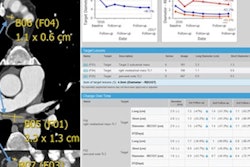
Example of metastatic lung lesion that became cavitary on the first CT following initiation of treatment. Most of the lung lesions in this patient became necrotic to the point of cavitation (commonly seen in this treatment) following the start of therapy. The lesions stayed the same size, however, and some measured larger on axial dimension. All images courtesy of Dr. Les Folio.After developing ADaVA to quantify changes in viable versus necrotic tumor volumes that are responding to antiangiogenic therapy, the researchers compared the ability of ADaVA, RECIST, and evolving criteria such as Morphology, Attenuation, Size, and Structure (MASS) and Choi. The study included 141 lesions at baseline and serial follow-up contrast-enhanced CT exams in 17 patients with metastatic bladder cancer being treated with cabozantinib, Folio said.
To provide a metric for treatment response, the researchers' method makes use of a PACS segmentation and density histogram partition tool that is included in Carestream's semiautomated Lesion Management application. The tool compares the change in the number of voxels corresponding to each density partition over serial exams.
"We segment the lesion and partition all HU densities by histogram within that lesion into ranges representative of viable, mixed, and nonviable [necrotic] tumor," Folio said.
In the 17 patients included in the study, ADaVA was the only tumor-response criteria to be significantly associated with overall survival, Folio said.
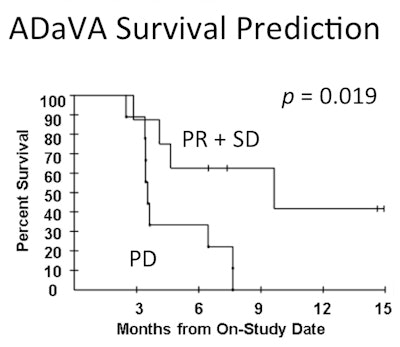 There was a statistical association between PD, PR + SD response determinations and overall survival (with binary tumor response) in total and low density-volume change in ADaVA (two-tailed, p = 0.019), compared with other criteria that showed weak or no association.
There was a statistical association between PD, PR + SD response determinations and overall survival (with binary tumor response) in total and low density-volume change in ADaVA (two-tailed, p = 0.019), compared with other criteria that showed weak or no association."Interestingly, volume alone was least effective in predicting overall survival," Folio said.
Broad applicability
The researchers believe their technique could broadly apply to all tumors. It would be particularly suited, however, to antiangiogenic and tyrosine kinase inhibitor treatments such as cabozantinib, which reduce metastatic lesion density with or without corresponding size change, Folio said.
"Direct volumetric lesion measurement in deformable organs seems to be a more appropriate and comprehensive method of assessing lesion size in serial exams," Folio said. "Use of full density assessment within each lesion volume also allows analysis of tumors that are not qualitatively necrotic but may show changes identifiable by software analysis."
The NIH research drew attention from oncologists at the ASCO meeting; many were not aware of the extent and availability of data within PACS, as well as the practicability of registration and automated segmentation as oncologic assessment tools, according to Folio.
"It seems that most oncologists have staff write down measurements, only to retype at least once to make them available for medical and research records," he said." Now we have a way to semiautomatically segment lesions, take into account the volume of presumed viable tumor, and manage response measurements within PACS, and [we are] currently researching the ability to export to clinical records and/or research databases. Coupled with improved tumor data management, criteria that are designed to fully utilize PACS segmentation advances pave the way for future automated tumor burden assessment."
Full density assessment within the lesion volume enables quantitative response assessment, which is more reproducible and objective. It also captures changes in tumor viability and composition, Folio said.
"We have been asked by several oncologists to apply this technique in various cancers treated with antiangiogenic therapies and have started to research this in sarcoma," he said.
The researchers are also beginning to test the ADaVA criteria in different tumor types, collaborating with other institutions to optimize response criteria and further automate and optimize software tools, Folio said. They would also like to extend the criteria to other modalities to assess functional change.
"One area of interest is studying how well density change correlates with FDG uptake by seeing whether areas of increased necrosis correspond with functional changes on PET/CT," he said. "Further study is needed to develop these criteria and improve segmentation tools; automated follow-up identification needs to mature before these types of assessment are ready for prime time."