Researchers at Houston Methodist Hospital are using a high-tech surgical planning room they call Plato's Cave to get the most out of their multimodality radiologic images. The Texas-sized cave helps surgeons prepare for their most challenging cases by revealing the anatomic relationships that are key to their decision-making.
Created for surgeons by surgeons, the 5D augmented virtual imaging environment combines PET, MR, and CT on multiple screens; multiple image-processing applications; and a large high-tech tabletop with a touchscreen. Its creator, radiation oncologist Dr. E. Brian Butler, said he started building the cave six years ago as something quite different -- a virtual patient project -- and that it morphed into its present role as a surgical planning tool.
Prehistoric wiring
Visualization is crucial in surgical planning and in life, according to Butler. Since prehistoric times, humans have been wired to respond to visual clues much better than other kinds of information, so the best way to improve surgical planning seemed to be the creation of a visual decision-making platform specifically dedicated to planning, he said.
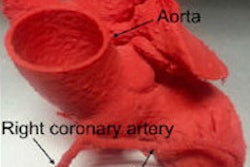
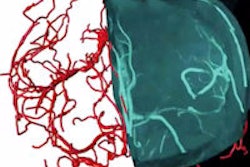
The team has approached this task with gusto. Plato's Cave takes DICOM images such as CT, MRI, and PET and performs reconstructions in 3D, 4D, and even 5D, according to Butler, who chairs the radiation oncology department at Houston Methodist and is also a clinical professor of radiation oncology at Weill Cornell Medical College.
"You can look at blood flow through the heart, or quantitatively measure the volume of a lesion in the lung, or fly through blood vessels," look at the inside, and measure their diameter, he said. "Not only do you have a picture, but you are flying into the picture and you're making measurements."
The room is highly visual and also interactive in a tactile sense. This occurs via multiple large displays and a jumbo touchscreen surgical table where four surgeons at a time can interact with images via hand gestures and voice commands. From there, they can virtually operate on patients before they get to the operating room, without the caution required in a sterile surgical room environment, Butler said.
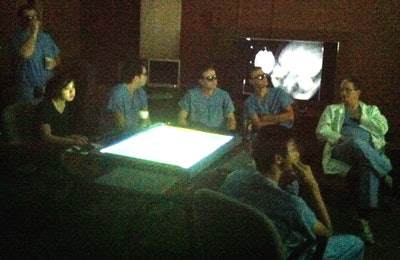 Dr. David Baskin (seated in lab coat at right) and residents review a case in the cave. Baskin is director of the neurosurgery residency training program at the Houston Methodist Hospital Neurological Institute, a professor of neurosurgery at Weill Cornell Medical College and Houston Methodist Hospital, and a professor of pharmacology and engineering at the University of Houston. All images courtesy of Dr. Brian Butler and Shirley Clark.
Dr. David Baskin (seated in lab coat at right) and residents review a case in the cave. Baskin is director of the neurosurgery residency training program at the Houston Methodist Hospital Neurological Institute, a professor of neurosurgery at Weill Cornell Medical College and Houston Methodist Hospital, and a professor of pharmacology and engineering at the University of Houston. All images courtesy of Dr. Brian Butler and Shirley Clark.In the cave, the surgeon finds the images that are most critical to the surgery and sends them digitally to the operating room. The patient's ID badge is recognized when he or she is wheeled into the room, and the relevant data and images are retrieved in preparation for the procedure.
The 25 x 25-ft cave was built from an old cobalt radiation therapy room, Butler said. It's equipped with a 16-ft screen, two projectors for a stereoscopic view and depth perception, and the touch table, all connected to a 3D printer.
"In that operating room, you can get a better perspective of what's really going on with the patient," Butler said. A lot of decisions made in surgery are based on whether a tumor encroaches on a blood vessel or some other anatomy. "For example, you can do a whole Whipple procedure before you did the Whipple procedure, look at all the blood vessels in three dimensions and fly through the blood vessels, and even record what you're doing."
Residents also benefit
Butler and his cave colleagues -- including Dr. Gavin Britz, chair of neurosurgery; Dr. Donald Donovan, chair of ear, nose, and throat surgery; and Dr. David Baskin, director of the neurosurgery residency training program -- think the cave has the potential to remake the way residents are trained.
To that end, they're setting up "minicaves" in the departments, such as one in otolaryngology, to help trainees prepare for the surgical suite. From these areas, they can explore the planning for every case going to surgery that day, using the library of complex cases as a teaching tool, Butler said. They can identify blood vessels and review key decision points, such as whether the tumor has invaded the superior mesenteric artery and how that affects pancreatic surgery planning.
Still on the wish list for trainees are haptic training methods to practice hands-on surgical techniques.
Like physicians, patients who visit the cave can relate better to 3D images than 2D, he said.
"They have this epiphany when they see where their disease is, and when you show it to them when it's gone, they really believe it," he said. And after surgery, patients can take home a CD of their own 3D images.
Commercial software for now
A lot of postprocessing software is built by computer people, Butler said, but he wants to assemble a unique platform that picks and chooses the functions that benefit surgeons specifically. At this point, the cave runs mostly on proprietary software, but the group is also developing its own.
The comprehensive vendor list for the cave includes dozens of familiar names, such as TeraRecon for postprocessing, "because it does some things a little better than the others," like extracting a liver, Butler said. But even the best software could be better tailored to surgeons' needs, and all of the graphical user interfaces could be stronger, he added.
The problem with radiology
Butler said pointedly that he can't rely on radiologists for surgical planning because they are "all trained in 2D" -- and generally deliver only 5-mm-thick images. Surgeons really need the raw 0.625-mm CT data to see what they're doing, he said.
"I spend most of my time yelling at radiology departments to give me all the data," he said. "Once I can get all the data, then the fidelity of the image and the reconstruction and the measuring is much better."
Things are different in the cave, he said. The amazing images and interactive capabilities "raise the playing field for all surgeons," not just the few with the intuition to look at a stack of CT images and reconstruct a 3D model in their heads, he said.
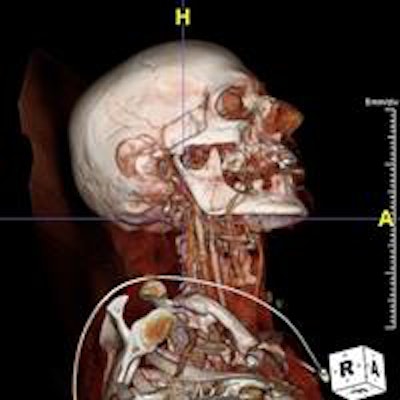
Meanwhile, the cave is reserved for the most complex cases, such as surgical planning for a man who tried to kill himself by shooting a crossbow in his mouth. The surgical team had to figure out how to remove the arrow without hitting the basilar artery or causing a cerebrospinal fluid leak, Butler recalled.
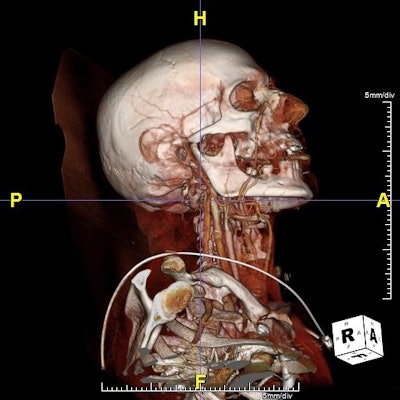 Patient was brought to a Houston emergency room with an arrow implanted in the area of the clivus. The arrow had been shot via crossbow. Dr. Mas Takashima, associate professor of otolaryngology and head and neck surgery at Baylor College of Medicine and associate professor of neurosurgery, performed a presurgical evaluation of the patient via the Plato's Cave interactive visualization platform. Takashima evaluated the optimal method to remove the arrow and prevent bleeding and potential cerebrospinal fluid leakage, finally removing the arrow without adversely affecting the patient, who is alive and doing well.
Patient was brought to a Houston emergency room with an arrow implanted in the area of the clivus. The arrow had been shot via crossbow. Dr. Mas Takashima, associate professor of otolaryngology and head and neck surgery at Baylor College of Medicine and associate professor of neurosurgery, performed a presurgical evaluation of the patient via the Plato's Cave interactive visualization platform. Takashima evaluated the optimal method to remove the arrow and prevent bleeding and potential cerebrospinal fluid leakage, finally removing the arrow without adversely affecting the patient, who is alive and doing well.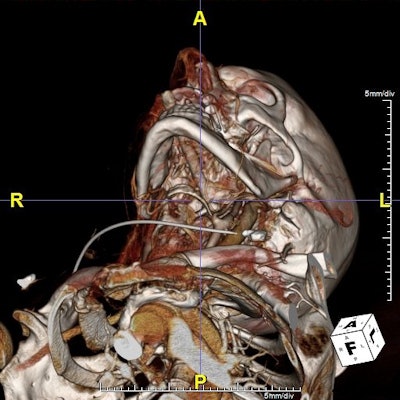
One exciting piece of software on hand maps the functional pathways in the brain in great detail. So when planning surgery to remove a brain tumor, surgeons can see how close they are to the functional speech pathway, whether the nerve fibers are serial or parallel, or whether there is redundancy in a tumor that spells a higher risk of recurrence.
"Knowing that information is enormous -- and we can take that data and superimpose it on our reference dataset and be able to understand the likelihood of causing some type of deficit," Butler said. You can't get it in a radiology report, he added.
The future promises even greater possibilities, with imaging incorporated into every operating room, according to Butler. Meanwhile, planning needs keep growing because surgery is being performed through smaller and smaller holes in the body.
Soon technology will allow doctors to create a coordinate system by tagging and labeling every structure in the body automatically and warning of nearby critical anatomy. Technology could someday allow the surgeon to "create a hologram of a patient, put on some haptic gloves, and reach inside the patient's body," he said. "It's theoretically possible."