Physical models of human anatomy created with 3D printing are finding a wide variety of uses, from medical education to surgical planning to forensic medicine. But what's the best way to get started with 3D printing -- without breaking the bank? Chinese researchers offer some guidance in an article in the International Journal of Computer Assisted Radiology and Surgery.
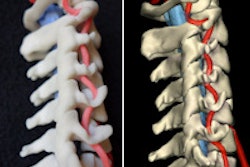
Based on a decade of experience, the group from Peking Union Medical College Hospital described methods for converting medical imaging data into 3D models of both hard and soft-tissue organs. The researchers used open-source software and a low-cost desktop 3D printer to reproduce digital and printed models of several anatomic targets, including teeth and dental pulp, the brain, and blood vessels.
"We have successfully converted multiple modalities of medical images to digital resources and printed models for both hard organs ... and soft-tissue organs," wrote Wuyang Shui and colleagues. "Three-dimensional printing (3DP) is a powerful tool to produce lifelike and tangible models" (Int J Comput Assist Radiol Surg, August 1, 2016).
Remaking medical education
Medical schools are coping with an ongoing shortage of donated cadavers for education and research, leaving trainees with few opportunities to work with actual organs.
 3D-printed skull. Image courtesy of Dr. Shi Chen.
3D-printed skull. Image courtesy of Dr. Shi Chen."Challenges faced by medical anatomy education include incomplete authenticity of traditional teaching materials, a limited number of donated bodies for dissection, and ethical issues," explained corresponding author Dr. Shi Chen in an email to AuntMinnie.com. "3D printing techniques solve those problems by constructing human anatomical structures within a short time and at low cost."
The group proposed the use of multiple modalities to create 2D and 3D resources, including volume-rendered images and digital models. Image data are acquired from subjects, and 2D and 3D resources including volume-rendered images and digital models are then created to supplement conventional training tools.
Volume rendering is useful for illustrating geometric structures and anatomic relationships with surrounding structures, but such images can only be viewed and not printed, the group wrote.
The right modality
Choosing the correct modality is key to enhancing contrast between the regions of interest (ROIs) and the surrounding structures, with the aim of minimizing the complexity, time, and cost of ROI extraction to digital media, they wrote. For example, CT is used to reconstruct the cranial base, and conebeam CT is used to reconstruct the tooth. MRI is favored for reconstructing brain and pituitary tumors, and CT angiography is the best choice for the heart chambers and vessel lumen, with medical images archived in standard DICOM format.
Volume rendering (VR) is effective for illustrating both the interior and the boundary of volume data with transparency and in various colors. Trainees can translate, rotate, and zoom the 3D images to view the details and anatomic relationships.
The open-source Visualization Toolkit (VTK) package was chosen to perform VR in real-time, integrating several volume-rendering algorithms. Both 3D texture-based volume rendering and ray-tracing tools are provided to perform VR.
Normally, three steps are used to build digital models from images: segmentation, reconstruction, and mesh processing. But segmentation is becoming optional as digital models can be generated directly using isosurface extraction. Still, the model will always emerge with extraneous triangle meshes and small holes that need mesh processing to improve accuracy and consistency. Once refined, the model is archived to stereolithography (STL) and printed.
Segmentation tools
Low contrast between the ROI and the surrounding images is challenging for creating models, so both the imaging modality and the segmentation algorithm should be chosen to maximize contrast. The authors chose the open-source Medicine Insight Segmentation and Registration Toolkit (ITK) software to develop segmentation tools that integrate threshold level sets, watershed, and region growing.
The automatic threshold segmentation tool is fast and effective for distinguishing the ROI from high-contrast images by setting a range of values, they noted. The ROI was extracted by comparing the density value of each pixel with a given threshold.
Having considered a range of printing techniques, the group chose the MakerBot Replicator 2 (MakerBot) and polylactide (PLA) filament materials for 3D printing. The deposition modeling printer uses a high-temperature nozzle to heat the PLA filament to a semiliquid state and print it one layer at a time.
After mesh processing is used to generate the digital model, it is imported to the MakerWare software, which is bundled with the MakerBot printer. The software performs translation, rotation, and scaling transformation to ensure that the printable model is aligned vertically with the top of the build plate and not outside of the printing space. The software automatically slices the digital model into layers, generating supporting structures on the build plate for construction, the authors wrote.
Qualitative assessment involves aligning the model in a common coordinate system while users watch and inspect the materials from different viewpoints. In quantitative assessment, a numerical tool is used to visualize any geometric deviation. Optical scanners enable highly accurate evaluation of dimensional errors by comparing the reconstructed model and corresponding scanned model using CloudCompare version 2.6.2 open-source software.
In the article, the authors described the following steps:
- The team produced multiple digital resources from medical images of living subjects.
- CT angiography images were used to create digital resources and printed models of the heart chambers and vessel lumen.
- Ray tracing was used to visualize the structure of the blood vessel from time-of-flight MR angiography images by setting the transfer function and color mapping.
"During the past 10 years, the application of 3D printing has been invaluable in anatomical training and surgical education, because it both avoids certain ethical concerns and provides more realistic educational resources," Shui and colleagues wrote. "3D printing is low in cost, high in accuracy, and involves a short production time. Multiple copies of dissected specimens and clinical case studies can be produced to scale in any size."
Studies have shown 3D-printed models to be more intuitive to use compared with digital models, and better able to capture complex 3D spatial relationships. The authors have submitted additional research for publication showing the value of 3D-printed models compared to conventional training, co-author Chen wrote in her email. For the new study, they designed a randomized controlled trial with 3D-printed skulls for anatomy education of medical students at the college.
"Our research showed 3D-printed skulls in this trial have certain benefits in basic cranial education over cadaveric skulls and atlases," Chen wrote. "In the future, we will use 3D-printed teaching visual aids in medical education and clinical medicine."