An Australian start-up firm called 4Dx has developed a new technique that combines fluoroscopy and advanced visualization to generate high-resolution images of lung-tissue motion and airflow. The firm hopes the technology will enable researchers to view and measure abnormal function in lung regions at the earliest clinical stages of disease.
Applied to chronic lung conditions such as asthma, cystic fibrosis, or chronic obstructive pulmonary disease (COPD), 4Dx hopes its technique will replace several pieces of diagnostic information from different sources that are currently needed to find out what's going on in the lungs, quickly assessing the patient's condition both qualitatively and quantitatively.
"The first applications are going to be in the regular follow-up of patients who have a chronic illness, and as they're undergoing treatment you can use the technology to see small changes early," said 4Dx President and CEO Dr. Andreas Fouras in an interview with AuntMinnie.com.
Measuring motion
4Dx's algorithm for turning the tissue measurements into lung motion analysis was first described in a 2012 paper by Fouras and colleagues Stephen Dubsky, Stuart Hooper, and Karen Siu in the Journal of the Royal Society Interface. Although the images in that paper were acquired using CT, 4Dx has settled on a process using fluoroscopy to convert breaths acquired at multiple time points to measure and depict airway motion, Fouras explained.
"The patients breathe under fluoro and we can record the motion of the tissues, and from that we can quantify a number of things, like ventilation," he said.
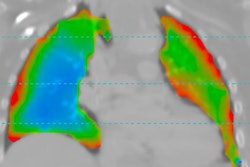
 Preclinical image of cystic fibrosis shows ventilation in an animal model using a fluoroscopy acquisition. All images courtesy of Dr. Andreas Fouras and Dr Rajeev Samarage.
Preclinical image of cystic fibrosis shows ventilation in an animal model using a fluoroscopy acquisition. All images courtesy of Dr. Andreas Fouras and Dr Rajeev Samarage.The paper describes lung inflation as a highly dynamic process involving multiple mechanical factors, including pressure gradients, tissue compliance, and airway resistance. The group devised a technique using fast synchrotron-based imaging at up to 60 frames per second that combines dynamic CT with cross-ventilation velocimetry to measure regional time constraints and expansion within the mammalian lung in vivo.
The method also estimates the airflow distribution throughout the bronchial tree during the ventilation cycle. An algebraic tomographic reconstruction is performed at each time point to yield a 4D movie of the lung morphology.
The authors calculated lung tissue expansion using a technique based on the discipline of particle image velocimetry, an approach routinely used in fluid mechanics studies to measure the velocity of tracer particles within a fluid flow. The process was designed for 2D but adapts easily to 3D. Dividing tissue displacement by the known time interval between frames yields velocity, a process to which lung tissue is well-suited as it consists of many air sacs, providing dense information for motion tracking.
Software is used to segment and track the bronchial tree and estimate airflow inside the tree. Assuming that air inside the lung and lung tissue is incompressible, the calculated lung expansion directly represents airflow into and out of the lung regions, the group explained.
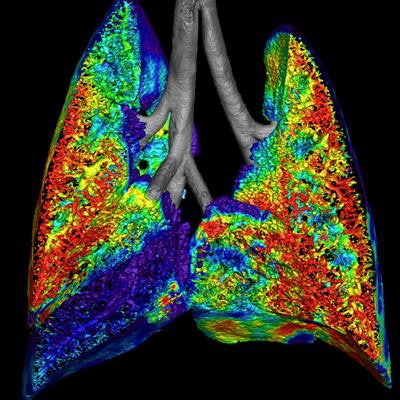
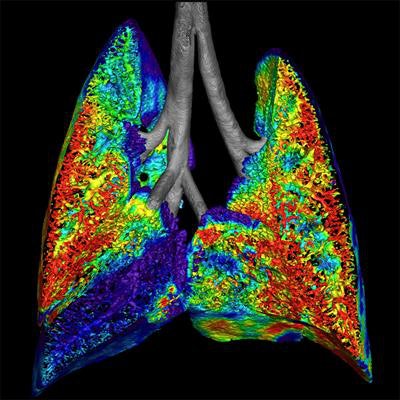
Preclinical data of regional airflow (colored) measured using 4Dx technology in healthy lungs (animal model).
4Dx's fluoroscopy-based technique, based on the same algorithm, aims to combine the best features of lung CT with spirometry to assess airflow in the patient, Fouras said. With CT, acquisitions are made at multiple time points and the 3D shape is reconstructed at those time points, while a similar process is performed in reverse order for the fluoro acquisitions that reconstruct motion rather than shape.
The software produces highly detailed maps of ventilation throughout the lung tissues, and it also draws color maps demonstrating airflow throughout the airway tree, whether measured directly from ventilation or from airway movement.
"We basically measure the motion first, and then from there we construct a 3D map of the motion from multiple views," Fouras said. "With fluoroscopy you can take a breath with the fluoroscopy looking at you from one view, and then you add two or more views and image the motion from other angles. Then you can reconstruct a 3D map of the motion."
The mathematics of reconstructing motion are very different from the mathematics of reconstructing shape, he added, and calculating motion allows the measurements to be completed with just three views -- fewer images than a comparable CT process. The radiation dose doesn't exceed 0.4 mSv for the fluoro exam. Any other imaging data that are available -- for example, from a prior CT scan -- can be used to reconstruct airflows for a more detailed picture of how air is flowing around the lungs.
How would it be used?
4Dx foresees a number of clinical applications for the exam. Cystic fibrosis patients, for example, frequently experience exacerbations of the disease and need regular follow-up that offers a lot of diagnostic information at a low radiation dose, Fouras said.
"Depending on the nature of the disease, it may be easier to see the disease through an image of the ventilation, or it may be easier to see it on the airways themselves where you can see the airflow going through," he explained. "It primarily depends on whether the disease is restrictive [affecting the tissues] or obstructive [affecting the airways]."
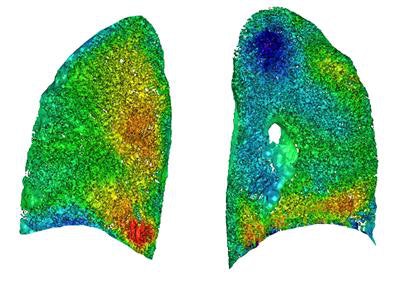 Image from a preclinical study of human lungs. The colors depict ventilation measured from the algorithm's viewpoint mapped onto CT.
Image from a preclinical study of human lungs. The colors depict ventilation measured from the algorithm's viewpoint mapped onto CT."We've been able to show that it's very powerful, not only for diagnosis, but more importantly for monitoring and follow-up of a patient as a disease progresses, or as a patient undergoes treatment," Fouras said.
Because the scan is quantitative, today's scan can be subtracted from last month's to quickly assess changes, a process that is less time-consuming and more accurate than a qualitative comparison.
"We show these as images, but underlying it all is hard data," he said, adding that airway motion is inextricably linked to air movement in and out of the lungs, and the 4Dx test measures lung motion directly.
As for alternatives to 4Dx's technology, there are technetium-based nuclear medicine studies and xenon gas CT exams, as well as MRI of hyperpolarized gases, "but what you're talking about in these studies is where that gas ends up over a period of time into the lungs, rather than where it's inhaled," he said. "This exam is closer to imaging the physiology, and it has some advantages in that it's completely contrast-free."
4Dx has found that its technology falls within 1% to 2% of spirometry results for measuring lung function, according to Fouras.
Toward clinical use
4Dx has tested the technology in animal studies and has started performing human studies.
"We've done a number of studies across a whole range of different diseases -- asthma, for example," Fouras said. "And we've done a whole range of diseases in mice and rabbits, and we feel like we're ready to be doing human subjects. We're not ready to publish the human studies yet, but we're very excited about how it's going."
Only about 25 humans and 500 mice and rabbits have been scanned to date using the fluoro technique, he noted, but a new study of 500 patients will substantially boost the numbers. 4Dx aims to submit its first 510(k) application to the U.S. Food and Drug Administration (FDA) by early 2017, involving use of the technique in patients who need frequent follow-up for chronic lung disease such as cystic fibrosis, lung transplant patients, or patients undergoing radiotherapy who may experience lung toxicity.
"Another thing that gives us a lot of confidence is that all the imaging we've done, all the results so far, show that the exam works the same way in people as it does in mice and rabbits," Fouras said. "The math behind it is the same."