Researchers are reporting positive results using a holographic augmented reality platform to assess splenic artery aneurysms (SAA) in a study presented at the Society of Interventional Radiology (SIR) 2018 annual meeting in Los Angeles.
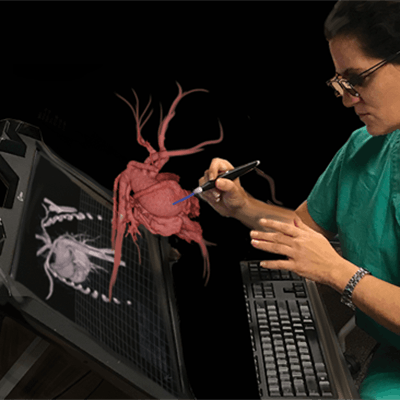
The researchers, led by Dr. Zlatko Devcic of Stanford University Medical Center, converted CT scans of several patients' splenic vasculature into holographic displays using software and a specialized workstation. They were able to move these images around in 3D as they searched for arteries associated with the aneurysms. Through the augmented reality platform, they were able to identify the correct arteries as accurately as they did when examining standard volume-rendered CT scans -- but with an added boost to reader confidence.
"This new platform allows you to view a patient's arterial anatomy in a three-dimensional image, as if it is right in front of you, which may help interventional radiologists more quickly and thoroughly plan for the equipment and tools they'll need for a successful outcome," Devcic stated in a press release.
Boosting reader confidence
The ongoing integration of virtual and augmented reality into healthcare has provided clinicians with a fresh outlook on human anatomy and pathology, which they, in turn, have been using to help improve patient care. The lifelike quality of virtual and augmented reality models has been especially valuable for physicians dealing with complex scenarios, such as separating conjoined twins, assessing fetal airway patency, and preparing for intricate procedures.
In that vein, the investigators of the current study set out to determine the effectiveness of using the EchoPixel platform to prepare for the minimally invasive endovascular repair of SAAs, which involves distinguishing the often-convoluted arrangement of arteries around the spleen.
"Treating splenic artery aneurysms can be very difficult because of their intricate nature and anatomic variations from patient to patient," Devcic noted.
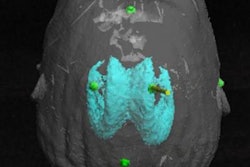
In the retrospective study, three radiologists tested an interactive holographic augmented reality platform (True 3D, EchoPixel). The True3D application takes data from CT and MRI scans, processes it with proprietary algorithms, and then outputs it to a 3D display. When users view the display with specialized glasses, volumes have the impression of floating in space and can be interrogated with a stylus as if they were real objects.
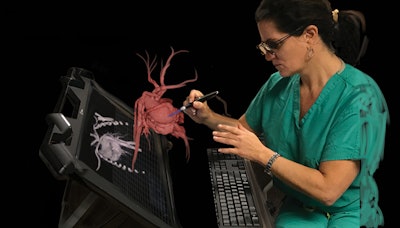 Physicians can examine medical images of vasculature as a holographic display through EchoPixel's True 3D augmented reality platform. Image courtesy of Dr. Zlatko Devcic.
Physicians can examine medical images of vasculature as a holographic display through EchoPixel's True 3D augmented reality platform. Image courtesy of Dr. Zlatko Devcic.The EchoPixel platform was compared to a conventional volume-rendering 3D workstation (AquariusNet Server, TeraRecon) for visualizing the CT angiography scans of 14 patients with SAAs. In these patients, 17 inflow and 22 outflow arteries were associated with 17 SAAs.
Through volume rendering, the radiologists were able to visualize the scans as 3D representations on a 2D screen, whereas the EchoPixel platform allowed radiologists wearing glasses to view patient's arterial anatomy as holographic displays and virtually manipulate them in an open 3D space.
The researchers found that the radiologists identified inflow and outflow arteries connected with the aneurysms just about as accurately with the holography platform as they did with the standard volume-rendering technique.
| Volume rendering vs. holography for evaluating splenic artery aneurysms | ||
| Volume rendering | Holographic augmented reality | |
| Accuracy | 88.9% | 89.7% |
| Sensitivity | 88.9% | 91.3% |
| Positive predictive value | 84.6% | 84% |
Using either method resulted in similar accuracies, sensitivities, and positive predictive values, but holographic augmented reality offered the additional advantage of increasing the radiologists' reading confidence; 93% reported an improvement (a score of 3 or 4 on a four-point scale) in confidence in their ability to spot arteries when using holography compared with the conventional method.
A different look
Augmented reality allowed the radiologists to view holographic displays of images as if they were real physical objects, providing them with information critical for endovascular repair of SAA, and, thus, significantly increasing operator confidence, according to Devcic.
"Preoperative planning is possibly the most important step toward successfully treating a patient, so the value of [virtual reality] cannot be understated," he said. "This technology gives us a totally different way to look at that structure and safely plan our approach to patient care."
Through this and future studies utilizing virtual and augmented reality, the researchers hope to confirm other potential clinical benefits of using the technology, such as reducing treatment time, radiation exposure, and contrast exposure.