Radiology residents who examined 3D-printed models of an acetabular fracture based on hip CT scans had a marked improvement in their understanding of the condition, according to an article published online recently in Academic Radiology. This could benefit the accuracy of their diagnostic reports.
The researchers, led by first author Dr. Omer Awan from Temple University Hospital in Philadelphia, created more than 50 3D-printed hip models of patients with different types of acetabular, or hip socket, fractures. They put these models on display for radiology residents during a lecture at their institution.
The residents who examined the 3D-printed hips had more than double the improvement in their knowledge- and diagnostic-based test scores than their peers who attended a similar lecture but did not have access to the models (Acad Radiol, July 30, 2018).
"These [3D-printed] models allow residents to understand the complexity of the spatial anatomy in a way that is superior to conventional lectures without the models," the authors wrote. "3D models pose an additional avenue for interactive learning that can help trainees retain complex information; which in turn, will help trainees' diagnostic acumen in formulating accurate diagnostic radiology reports."
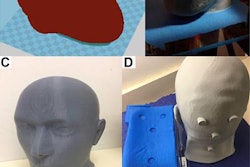
 Color-coded 3D-printed hip model with an acetabular fracture. Image courtesy of Dr. Omer Awan.
Color-coded 3D-printed hip model with an acetabular fracture. Image courtesy of Dr. Omer Awan.Improving resident understanding
The application of 3D printing in medicine has predominantly centered on improving patient outcomes -- including lowering surgical times and costs -- by allowing physicians to plan and simulate interventional procedures such as ultrasound-guided femoral artery access and stroke clot removal. Clinicians are also increasingly using 3D-printed models during patient consults to help patients better understand their condition and possible treatment options.
A less common use has been to bolster radiologists' anatomical knowledge with 3D-printed models to ultimately increase their diagnostic accuracy, the authors noted.
Looking to explore the potential benefits of 3D printing for radiologic diagnosis, Awan and colleagues obtained CT scans of patients with five of the most common types of acetabular fractures and then used these scans to create 55 hip models via 3D printing. They constructed the 3D-printed hips by converting the CT scans into virtual 3D models using volume-rendering software (TeraRecon), editing these files with open-source software (Meshmixer, Autodesk), and finally printing the models with a 3D printer (Dimension Elite, Stratasys).
The cost to print a 1-to-1 scale model was between $100 and $200, and it took approximately 36 to 48 hours for printing, postprocessing, and drying. The researchers additionally painted various parts of the model in different colors to simplify the identification of key structures.
After creating the models, the researchers prepared two versions of a musculoskeletal radiology lecture covering acetabular fractures: One presentation displayed 3D-printed models with x-ray and CT scans and the other only showed the medical images. Among 22 radiology residents who signed up for the lecture, half attended the version that included 3D-printed models and half attended the version showing only medical images.
The residents completed a test immediately before the lecture and again three weeks after the lecture. The test included various questions concerning the diagnosis of acetabular fractures on x-ray and CT scans.
Enhancing radiologic diagnosis
On average, both groups of radiology residents had considerably higher scores on their post-test than they did on their pretest. However, there was a statistically significant difference (p = 0.04) in the improved scores between residents who had access to the 3D-printed hips and those who did not. Residents who examined the 3D-printed hips had a 35.5% improvement on their exam scores, compared with a 16.4% improvement for residents who did not see the models.
| Radiology resident education with 3D-printed models vs. without | ||
| Musculoskeletal lecture without 3D-printed models | Musculoskeletal lecture with 3D-printed models | |
| Mean score on pretest | 39.1% | 36.4% |
| Mean score on post-test | 55.5% | 71.8% |
| Median score on pretest | 40% | 40% |
| Median score on post-test | 50% | 70% |
Residents who studied 3D-printed models had markedly higher post-test scores than their peers who did not look at the models. This suggests that 3D printing can enhance short-term learning outcomes in radiology trainees and may be a useful educational tool for mastering acetabular fracture classification, Awan and colleagues noted.
"Some institutions may be apprehensive in adopting 3D models in their educational pedagogy, given the relatively high financial costs of printing the models," they wrote. "[But] more cost-effective 3D imaging software does exist and have been used in teaching complex anatomy to students."
Though the results strongly favor implementing 3D printing into radiology education, the investigators acknowledged that the study was limited by its small population size and the potential, albeit subtle, for observer bias from having the same faculty member present at both lectures.
"Further studies would be necessary to assess long-term learning outcomes with larger sample sizes in multiple radiology residency programs to elucidate the effect of 3D models," they wrote. "3D models could also be applied to facilitate learning additional complex radiology topics."