CHICAGO - Virtual reality (VR) and augmented reality (AR) technologies offer an interactive, 3D visualization of brain cancer that can help improve preoperative planning and intraoperative guidance for brain tumor resection, according to a Tuesday presentation at RSNA 2018.
The researchers, led by presenter Dr. Vinodh Kumar from MD Anderson Cancer Center, investigated the potential clinical applications of VR and AR for evaluating and treating adult cerebral hemispheric glioma. They found that examining brain and tumor anatomy within the fully immersive 3D virtual environment of these technologies greatly enhanced radiology image review, particularly for presurgical planning.
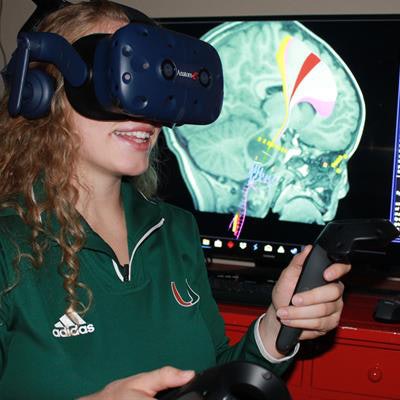
 A virtual reality device allows users to visualize 3D images of patients' brain MRI scans. Image courtesy of Dr. Vinodh Kumar.
A virtual reality device allows users to visualize 3D images of patients' brain MRI scans. Image courtesy of Dr. Vinodh Kumar."It is no longer adequate to analyze complex brain and skull-base tumors on 2D flat monitors," Kumar told RSNA attendees. "The future of neuroradiology is in advanced techniques such as virtual reality and augmented reality, which produce a dynamic, interactive 3D view of the patient's imaging."
Dynamic, interactive visualization
Hoping to take advantage of the enhanced 3D visualization of VR and AR, Kumar and colleagues acquired the MRI scans of glioma patients from a database of approximately 1,250 cases and sent the anonymized scans to an independent virtual reality technology company. The company processed the scans into 3D virtual models that were compatible with virtual reality software (Radiolog-e, Anatom-e Information Systems).
 Dr. Vinodh Kumar.
Dr. Vinodh Kumar.The researchers then put on a VR headset to examine the 3D brain and glioma images in a realistic and immersive simulation. They were able not only to look at the images in a 3D environment but also to alter their orientation using two advanced joysticks -- including dynamically zooming in and out of images.
This VR-based visualization enabled neuroradiologists to map out the intricate gyral anatomy of the brain, surrounding vasculature, and tumor infiltration patterns much more effectively than they could by looking at standard MRI scans on a 2D screen.
In this way, the technique could be particularly useful during presurgical planning for brain tumor resection, Kumar noted. It also has the potential to help improve patient education during consults before surgery, as well as assist in medical training and interdisciplinary meetings among clinicians.
Thus far, the group has confirmed the technology's feasibility in retrospective analyses of real clinical cases. In one such case, VR helped the researchers see that a fiber tract known as the posterior arcuate fasciculus ran through the brain tumor -- a crucial detail they missed when examining diffusion-tensor MRI scans. The neuroradiologists shared this information with their neurosurgical colleague, who then used this knowledge for surgery.
"We feel that in the future, once the technology reaches U.S. Food and Drug Administration approval, virtual reality will have much more widespread clinical use," he said.
For the retrospective tests, Kumar collaborated with Dr. Jill Hunter from Texas Children's Hospital and Dr. Komal Shah, Dr. Maria Gule, Dr. Melissa Chen, Dr. Halyna Pokhylevych, Dr. Donald Schomer, and Dr. Anne Hayman from MD Anderson Cancer Center.
Future of neuroradiology
More recently, Kumar and colleagues have been working on increasing the viability of AR for preoperative planning in cases involving complex brain tumors. They reported that AR was superior to VR in anatomy and tumor display.
It also allowed for multiple clinicians wearing AR glasses to view 3D images of the brain and gliomas simultaneously, Kumar noted. This feature makes it more valuable for communication between radiologists and neurosurgeons, compared with the single-user limitation of VR headsets. Radiologists could also use AR to record their interpretation of images in a video and send that audio and visual display to surgeons, who could assimilate the information more quickly than with a traditional radiology report.
Furthermore, AR has the potential for intraoperative use by fusing holographic models of MRI and CT scans directly onto the patient's anatomy during neurosurgery or spinal surgery, he noted.
"At this time, VR is superior to AR, as it is better established and a stable platform," Kumar said. "However, as technology advances, AR will likely overtake VR for preoperative planning of brain tumors."
Kumar highlighted several key advantages of using VR and AR in the management of complex brain tumor cases:
- The 360° view of 3D images bolsters radiological interpretation.
- VR and AR can reveal structures at high risk of injury during surgery or radiotherapy.
- They can help clinicians explain medical procedures to patients more clearly -- improving patient satisfaction.
- They allow for a more effective use of imaging before and during procedures.
"Both VR and AR are innovative alternatives to conventional 2D imaging for preoperative planning of complex glioma cases," he said. "The continued development of both of these technologies is needed to advance neuroimaging."



















