Cinematically rendered CT images allowed clinicians to understand patient anatomy more quickly and with a greater degree of accuracy than conventional CT, according to an article recently published online in JAMA Surgery. Researchers from Germany suggest the technique may also benefit surgical planning and decision-making.
The group from Friedrich-Alexander University of Erlangen-Nürnberg compared the ability of surgeons to perceive aspects of patient anatomy critical for the surgical management of hepatopancreatobiliary tumors on standard CT scans versus cinematically rendered CT scans. The researchers found that cinematic rendering enabled the surgeons to complete the task with higher accuracy in roughly half the amount of time (JAMA Surg, May 29, 2019).
"Surgeons perceive cinematic rendering imaging as a helpful tool that not only promotes their anatomical understanding but may also enhance preoperative and intraoperative decision-making," lead author Dr. Moustafa Elshafei and colleagues wrote.
Cinematic rendering vs. CT
Surgical decision-making relies heavily on an operating clinician's grasp of patient-specific anatomy, which is based in large part on medical imaging data. Though generally sufficient for displaying basic structures, standard 2D imaging offers a restricted view of complex anatomy that often demands advanced spatial reasoning skills.
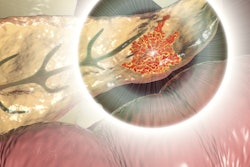
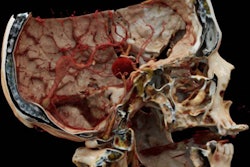
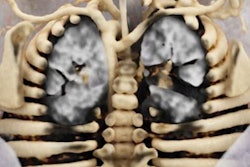
In search of a more intuitive visualization technique, numerous groups have turned to volume rendering and, more recently, cinematic rendering -- a 3D visualization method that deploys global light maps to produce highly detailed and shadowed images. Several preliminary studies have demonstrated the capacity of cinematic rendering to provide photorealistic depictions of intricate, highly vascularized organs such as the spleen and liver.
But to what extent does the photorealism of these cinematically rendered images improve clinicians' understanding of complex anatomy?
To answer this query, Elshafei and colleagues applied a proprietary cinematic rendering technique to the abdominal CT scans of 40 patients who had received treatment for hepatopancreatobiliary tumors at their institution from 2015 to 2017. (The cinematic rendering software application the group used is a prototype that is still pending approval for clinical use.)
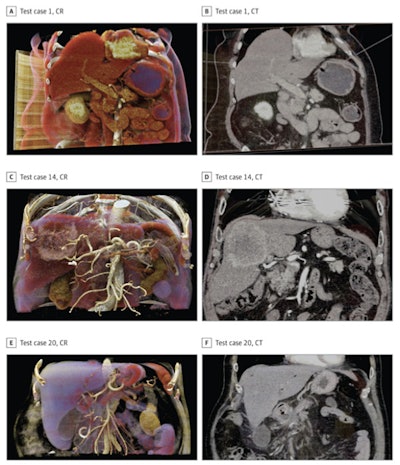 Cinematically rendered images (left column) juxtaposed with corresponding CT scans (right column) of pancreatic (A-B) and liver (C-F) anatomy. Images courtesy of Elshafei et al. Licensed under CC BY 4.0.
Cinematically rendered images (left column) juxtaposed with corresponding CT scans (right column) of pancreatic (A-B) and liver (C-F) anatomy. Images courtesy of Elshafei et al. Licensed under CC BY 4.0.A total of 18 resident and attending surgeons used either the conventional CT scans or cinematically rendered CT images to complete an assessment concerning essential facets of patient anatomy in the context of preoperative planning and intraoperative strategies. Those who examined the conventional CT scans first also examined the cinematically rendered images following a two-week washout period, and vice versa.
Overall, cinematic rendering was associated with a better understanding of patient anatomy, compared with conventional CT, regardless of the type of imaging data the surgeons looked at first.
The surgeons' assessment scores were 8.5 percentage points higher for cinematic rendering than they were for CT, when they had access to the cinematically rendered CT scans right away (CR-CT). The difference increased to 13.1 percentage points when the physicians examined the cinematically rendered CT scans after first seeing the conventional CT scans (CT-CR).
| CT vs. cinematic rendering for understanding patient anatomy | ||
| CT | Cinematic rendering | |
| Accurate identification of patient anatomy (CR-CT) | 90.2% | 98.7% |
| Accurate identification of patient anatomy (CT-CR) | 86.6% | 99.7% |
| Time required to complete assessment (CR-CT) | 75 seconds | 56.6 seconds |
| Time required to complete assessment (CT-CR) | 95.1 seconds | 42.7 seconds |
Cinematic rendering helped clinicians answer anatomy-related questions more quickly and accurately than CT, suggesting that the advanced visualization technique may enhance their understanding of complex anatomical information during presurgical planning, according to the authors.
'One step closer'
Following the assessment, the clinicians also completed questionnaires rating the utility of cinematic rendering. The consensus was that the technique was "beneficial for the comprehension of the surgical anatomy," especially regarding vascular anatomy and spatial relationships among structures.
Most of the surgeons also agreed that cinematic rendering could be helpful for interdisciplinary decision-making, intraoperative guidance, and informed consent discussions. However, these claims were entirely subjective, and it remains to be determined whether clinical use of cinematic rendering actually improves surgical decision-making and patient outcomes, the authors noted.
"The other, parallel story in this article is that the technology had no [statistically] significant association with intraoperative decision-making or patient communication, further distancing any real return on investment as a teaching tool for students and residents," Dr. Carla Pugh, PhD, of Stanford University wrote in an accompanying editorial.
What's more, the relatively modest increase in accuracy regarding anatomical understanding, though statistically significant, still might not be enough to justify the additional labor or cost involved with employing cinematic rendering and similar 3D imaging techniques on a regular basis, Pugh continued.
"We are still far away from wide adoption and widespread use of these techniques in the operating room for all specialties," she wrote. "With cinematic rendering as one of the newer 3D reconstruction techniques, we may be one step closer to achieving lifelike representations of imaging data and enhancing diagnostic utility; however, there is still more work to be done."