Where standard methods to reconstruct damaged chest walls fall short, 3D printing may offer a hopeful alternative, according to researchers from the Mayo Clinic. They demonstrate several benefits of using a 3D-printed model to plan chest wall surgery in an article published in the August issue of Trauma Case Reports.
"Chest wall reconstruction can be challenging, fraught with difficulties. ... Meticulous surgical planning is essential for the achievement of optimal outcomes," corresponding author Dr. Brian Kim and colleagues wrote. "The advent of accessible, hospital-based 3D modeling can facilitate preoperative understanding of the underlying anatomy and optimize surgical planning."
The group demonstrated the benefits of integrating 3D printing into preoperative planning for surgical stabilization of rib fracture in a 55-year-old man. The patient had undergone surgery for a stab wound in his left chest wall two months prior to presenting to the current hospital with nonunion, a serious complication of failed fracture repair (Trauma Case Rep, August 2019, Vol. 22, 100218).
Due to the complexity of the case and concerns over future nonunion, the researchers decided to plan the repair of the patient's chest wall using a 3D-printed model. To make the model, they acquired chest CT scans of the patient, segmented the scans using computer software, and converted the scans into virtual 3D models. Then they exported the 3D models as stereolithography (STL) files into a 3D printer (Objet 500, Stratasys) in order to create a patient-specific 3D-printed chest wall.
Kim and colleagues studied the lifesize, multicolor 3D-printed model to orchestrate their surgical approach. The model also enabled the surgeons to easily understand the patient's anatomy and regions most susceptible to complications, as well as provided them a realistic model on which to practice cutting and reshaping the bones.
Of note, a thorough examination of the 3D-printed model directed the surgical team's attention to a particular joint between the rib and sternum that required stabilization repair before placement of the metal plates and screws. This was a critical observation that would have likely gone unnoticed with conventional planning on CT scans or virtual 3D models, according to the researchers.
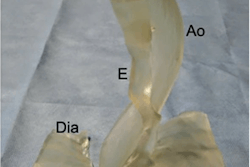
 3D-printed model of the chest wall demonstrating a nonunion of the costal cartilage in a 55-year-old man. Image courtesy of Bergquist et al. Licensed under CC BY 4.0.
3D-printed model of the chest wall demonstrating a nonunion of the costal cartilage in a 55-year-old man. Image courtesy of Bergquist et al. Licensed under CC BY 4.0.In addition, having access to the 3D-printed model allowed the surgical team to preoperatively shape metal plates, which they later used during surgery to stabilize the chest wall, to the patient's specific anatomy. This process helped the team to avoid spending a considerable amount of time contouring and then sterilizing the plates during the operation.
Follow-up CT scans of the patient showed good alignment and resolution of the patient's initial complaints of pain and difficulty breathing.
One of the barriers to medical 3D printing continues to be its high cost, but the technology's capacity to bolster presurgical planning, decrease operating times, and possibly reduce the need for follow-up operations could make up for the initial cost. What's more, clinicians now also have the option to request reimbursement with the new Current Procedural Terminology (CPT) category III codes in place as of July.
"We believe that the early adoption of this technology by surgeons can help improve surgical quality and provide more individualized patient care," the authors wrote. "Centers should pursue the integration of 3D-printed models into their practice, and active collaborations between surgeons and modeling experts should be sought at every available opportunity."