Researchers from Australia have created a 3D-printed head model, based on a combination of MRI and CT angiography scans, that allows for the realistic simulation of neurosurgical procedures. They discuss the specifics of their method in an article published online August 1 in 3D Printing in Medicine.
Simulation is widely regarded as a core part of training for complex neurosurgical procedures such as cerebral aneurysm repair, which requires a specialized skill set and high proficiency with microinstruments, noted the authors, led by Ruth Nagassa from Monash University in Australia.
A shortcoming of most current simulation-based training techniques, however, is that they rarely involve simulating procedures in their entirety or offer meaningful tactile feedback, the authors continued. One possible answer to this need may be to create neurosurgical simulation models from medical imaging data using 3D printing technology.
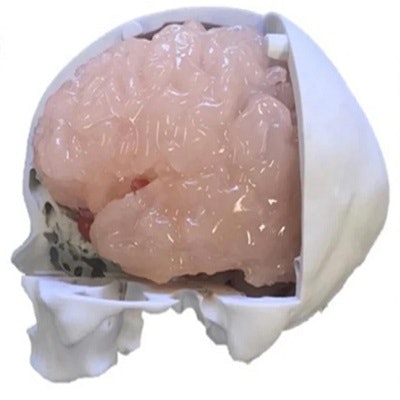
The researchers thus set out to create a model for simulating cerebral aneurysm repair that consisted of a combination of various generic and patient-specific 3D-printed anatomical parts, including individually printed models of the skull, skin, brain, meninges, cranial nerves, and vasculature.
They began by obtaining the CT angiography scans of a patient who presented with a middle cerebral artery aneurysm greater than 5 mm. They generated a virtual 3D model of the scans, from which they segmented and edited the three main cerebral arteries using computer software.
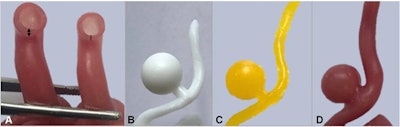 A: 3D-printed model of the middle cerebral artery composed of three layers of silicone (double-sided arrow) and two layers of silicone (single line). B, C, and D: 3D-printed model for simulating cerebral aneurysm repair. All images courtesy of Nagassa et al and licensed under CC BY-NC 4.0.
A: 3D-printed model of the middle cerebral artery composed of three layers of silicone (double-sided arrow) and two layers of silicone (single line). B, C, and D: 3D-printed model for simulating cerebral aneurysm repair. All images courtesy of Nagassa et al and licensed under CC BY-NC 4.0.After processing, they input the virtual models into a desktop 3D printer (Form 2, Formlabs) and used wax and silicone to produce the 3D-printed vasculature. The final model had differing layers of silicone applied to the vascular wall to ensure an accurate representation of varying vessel wall thickness, depending on the extent to which a region was affected by an aneurysm.
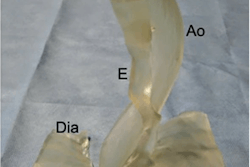
Next, Nagassa and colleagues created a generic head model into which they inserted the patient-specific 3D-printed vasculature. The generic component comprised a 3D-printed skull based on CT scans of a cadaver, 3D-printed brain and meninges based on T1-weighted MRI scans of a patient, 3D-printed cranial nerves based on dissected specimens, and 3D-printed facial skin.
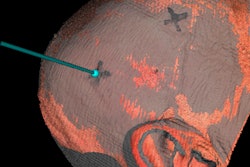
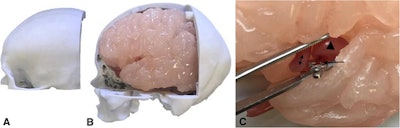 Patient-specific 3D-printed model for neurosurgery simulation, including a 3D-printed skull, brain, and artery with an aneurysm (arrowhead).
Patient-specific 3D-printed model for neurosurgery simulation, including a 3D-printed skull, brain, and artery with an aneurysm (arrowhead).After constructing the 3D-printed anatomical models, the researchers obtained linear and volumetric measurements of the models and compared them with measurements from the original medical imaging data. Quantitative evaluation of these values showed relatively minor variation between the original imaging data and the 3D-printed models.
To be specific, they found that the correlation coefficient between the 3D-printed models and the original data was between 90.2% and 99%, depending on the body part, with an overall percentage difference of less than 0.4% -- confirming the structural accuracy of the models. In addition, the vessel wall thickness of the healthy 3D-printed arteries (0.52 mm) matched the thickness of typical vessel walls (0.5 mm to 0.7 mm).
What's more, the type of materials used to create the 3D-printed aneurysm repair model replicated the textural properties of actual human tissue, allowing for realistic surgical simulation from start to finish, the authors noted. The manufacturing cost of the entire simulation model was approximately $1,280 and took 40 hours to complete.
Though expensive and time-consuming, nearly all of the model components are reusable and interchangeable, and they may be applicable for a variety of endovascular procedures performed by surgeons and interventional radiologists, the authors wrote.
"Further assessment of our simulator with neurosurgical trainees will be essential to assess the endovascular applications of the simulator," they concluded. "Our simulator could easily be adapted for aneurysms in other sites such as the anterior communicating artery."