A new technique that relies on 3D-printed surgical guides designed with CT data enhanced the accuracy of total knee replacement procedures and also decreased postoperative bleeding and trauma, compared with the standard technique, in a study published online on February 22 in Orthopaedic Surgery.
The effectiveness of total knee arthroplasty, or knee replacement, hinges largely on the precision of knee joint measurements that can vary in individuals with degenerating conditions such as advanced knee osteoarthritis. Rather than obtain patient-specific measurements, however, surgeons use generic measurements for traditional knee arthroplasty. As a result, roughly 35% of patients who undergo traditional total knee arthroplasty request a revision procedure within the first two years.
In recent years, clinicians have sought out more personalized approaches to knee replacement procedures in order to better meet the actual needs of patients. The most common approach, called patient-specific instrumentation, uses surgical guides based on 3D CT or MRI data to help individualize knee replacement procedures.
For the current study, Dr. Rui He and colleagues from Third Military Medical University in China explored the potential benefits of applying 3D printing technology to patient-specific instrumentation for 80 patients with advanced knee osteoarthritis. Half of them underwent traditional knee arthroplasty and the other knee arthroplasty with patient-specific instrumentation using 3D-printed surgical guides.
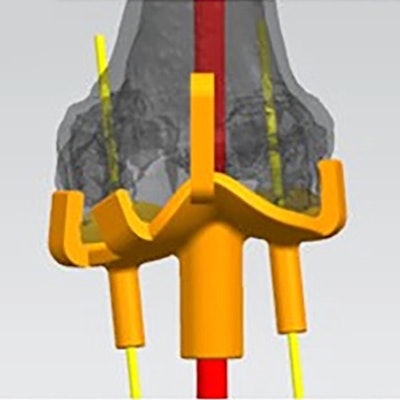
To create the guides, the researchers imported the patients' CT scans into 3D image processing software, converted the scans into virtual 3D knee models, and produced the surgical guide using a 3D printer (UpBox, TierTime). They designed the models to include entry points and a positioning hole for surgical guidance.
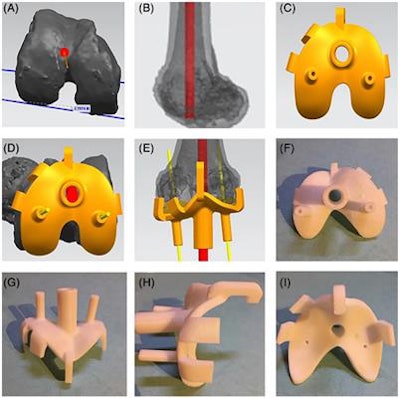 The workflow for creating patient-specific instrumentation using 3D CT data (A-E) and 3D printing technology (F-I). Image courtesy of He et al and licensed under CC BY-NC 4.0.
The workflow for creating patient-specific instrumentation using 3D CT data (A-E) and 3D printing technology (F-I). Image courtesy of He et al and licensed under CC BY-NC 4.0.For both the 3D printing and conventional treatment groups, the total knee arthroplasties resulted in statistically significant improvements in knee condition (p < 0.05), based on several follow-up clinical and radiological evaluations. There were no major differences between the two groups in terms of the knee range of motion and the amount of time it took to drain it after surgery.
The researchers did find that the 3D printing method led to considerable reductions in postoperative bleeding; the 3D printing group had 258.7 mL of postoperative fluid drained on average, compared with 305.6 mL for the conventional group (p < 0.05).
Surgery with the 3D printing method was also much more accurate, as indicated by better rotational alignment around the knee joint. For example, measurements of the posterior condylar and patella transverse axis-femoral transepicondylar axis angles were better (i.e., closer to 0°) for the 3D printing group than the conventional group (p < 0.05).
In addition, the depth of the intramedullary guide inserted during surgery was significantly smaller in the 3D printing group at 9.4 cm than in the conventional group at 20.4 cm (p < 0.001), where a smaller depth is considered less invasive and indicates less trauma.
The downside of the 3D printing technique, however, was that it required a longer average operating time of 87.3 min, compared with 73.6 min for the conventional technique (p < 0.001), and increased operational costs.
"3D printing-designed patient-specific instrumentation could assist in [placement of] the intramedullary guide and align femoral rotation more accurately compared with traditional total knee arthroplasty to obtain satisfactory short-term clinical efficacy," the authors wrote.



















