Researchers from Tennessee have developed a navigation technique that employs a 3D light scanner and 3D printing technology to improve the accuracy and workflow of minimally invasive procedures reliant on CT data. They describe their technique in an article recently published in World Neurosurgery.
Management of subdural hematomas typically entails a minimally invasive procedure called subdural evacuation port system (SEPS) placement that takes place at the patient bedside. The procedure requires neurosurgeons to drill a burr hole at the thickest part of the hematoma, which they usually identify preoperatively by examining CT scans.
The standard CT-based method for determining SEPS placement is challenging, however, given the difficulty of matching visible surface landmarks on a patient's head with CT scans, lead author Dr. Hansen Bow, PhD, from Vanderbilt University told AuntMinnie.com.
Seeking to improve upon this traditional method, Bow and colleagues conducted a pilot study in which they explored the potential of using light-based 3D scanning to identify the optimal location for making burr holes (World Neurosurgery, February 4, 2020).
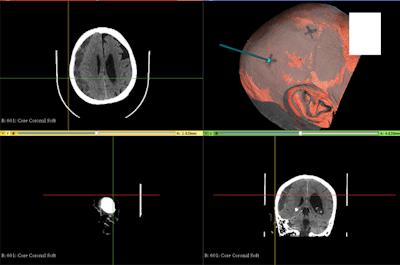
The researchers tested their 3D scanning technique on a 3D-printed head model, which they generated using CT data. The 3D scanning technique involved projecting light patterns from a multimedia projector onto the 3D-printed head and capturing the patterns with a camera. An algorithm then used these light patterns to generate a virtual 3D model of the head.
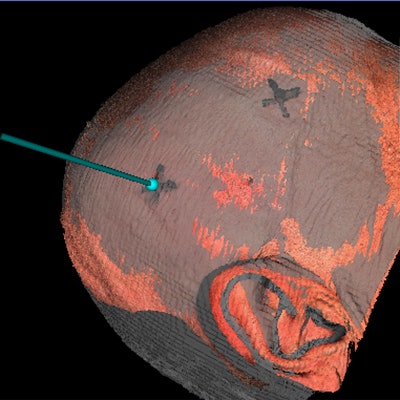
 A color 3D reconstruction (top right) based on a patient's head CT scans, with an "X" indicating the proposed site for SEPS placement. Image courtesy of Dr. Hansen Bow, PhD.
A color 3D reconstruction (top right) based on a patient's head CT scans, with an "X" indicating the proposed site for SEPS placement. Image courtesy of Dr. Hansen Bow, PhD.Finally, the researchers registered the virtual 3D model to CT scans of the 3D-printed model to determine the ideal entry point for SEPS placement. They tested their technique 10 times and calculated an average registration error of less than 2 mm, confirming the accuracy of the method.
Following the success of these early tests, the researchers applied their 3D navigation technique to five SEPS placement procedures for patients requiring chronic subdural hematoma evacuation. Obtaining an accurate 3D light scan of a patient's head using the technique took an average of 1 to 2 minutes.
Overall, Bow and colleagues found that the new 3D navigation technique was highly accurate at suggesting the optimal site for SEPS placement. The average distance between the anticipated SEPS burr hole location (based on registration of the virtual 3D model to CT scans) and the actual burr hole location was less than 1 cm, which falls within the acceptable error limit for SEPS placement.
"Using light-based 3D surface scanning and image registration to a preprocedure head CT, neurosurgeons may be able to more accurately select where to drill burr holes as part of a bedside procedure," Bow said.
Continued refinement of the 3D navigation technique will enable surgical trainees to perform bedside procedures more efficiently without the need to rely on CT scans to guide optimal SEPS placement, ultimately decreasing costs attributed to imprecise placement, he said.