3D-printed models based on CT scans not only facilitated presurgical planning for kidney cancer removal but also enhanced navigation during surgery, ultimately reducing patient blood loss in a new study, published online July 21 in the Journal of International Medical Research.
Researchers from China compared the outcomes of kidney-sparing surgery for more than 100 cancer patients who underwent the procedure either with or without the assistance of 3D printing technology.
"Compared with conventional 2D radiographic images, 3D-printed physical anatomic models are intuitive, capable of 3D representation, and easy to understand; therefore, they can aid surgeons in preoperative planning and intraoperative navigation," study co-author Dr. Yu Xie of Hunan Cancer Hospital in Changsha and colleagues wrote.
They found that individually tailored 3D-printed kidneys proved to be valuable tools in preparing for and guiding kidney tumor surgery -- contributing to sizeable reductions in blood loss and rate of surgical complications.
Addressing complex surgery
"Research regarding 3D-printed physical anatomic models has shown that they improve understanding and characterization of kidney anatomy in both patients and medical students," the authors wrote. "Importantly, 3D printing techniques bridge the gap between imaging and actual anatomy, providing a more tangible method for evaluation and comprehension of pathology."
The various advantages that 3D printing affords are particularly useful for managing challenging cases such as partial nephrectomy, or kidney-sparing surgery, which is a minimally invasive procedure for removing kidney cancer. The procedure is associated with a high rate of surgical complications due in large part to the need to temporarily suspend blood supply to the kidney during surgery, a process referred to as warm ischemia.
In order to decrease the risk of surgical complications, Xie and colleagues explored a new technique using 3D printing to assess 127 patients who underwent kidney-sparing surgery between January 2016 and February 2018 (J Int Med Res, July 21, 2019).
The surgical team used patient-specific 3D-printed kidneys to aid preoperative surgical planning and intraoperative navigation for roughly 54% of the patients; the rest of the patients received traditional surgical treatment with CT scans for planning and navigation. The researchers cited no notable differences between the groups in terms of the patients' age, sex, tumor size, or tumor complexity score based on the RENAL nephrometry scoring system.
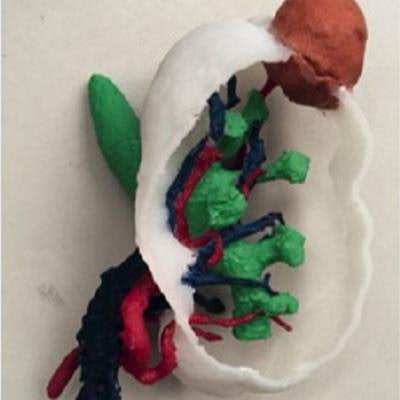
For the 3D printing patient cohort, the researchers processed the patients' CT scans using computer software (Mimics 18, Materialise) and then created multicolor 3D-printed kidneys, with distinct anatomical structures represented by different colors. After production, a team of radiologists and urologists confirmed the accuracy of the dimensions of each model in comparison with the original patient anatomy.
 3D-printed kidney based on patient CT scans. The model displays the segmental arteries and veins (red, blue), renal pelvis (green), and renal mass (salmon pink). Image courtesy of Fan et al. Licensed under CC BY-NC 4.0.
3D-printed kidney based on patient CT scans. The model displays the segmental arteries and veins (red, blue), renal pelvis (green), and renal mass (salmon pink). Image courtesy of Fan et al. Licensed under CC BY-NC 4.0.The same team subsequently used the 3D-printed models to discuss the feasibility of various surgical techniques, identify potential complications, and finally decide on the ideal surgical approach. During surgery, a surgical assistant aligned the 3D-printed model for each case with the laparoscopic display to help the operating surgeon quickly identify the tumor's location.
Postoperative exams revealed that the tumor margins were cancer free for all of the patients, regardless of the surgical technique employed.
Improved planning, outcomes
Overall, the 3D-printed models helped surgeons fully understand the spatial relationships between kidney structures during presurgical planning and accurately locate tumors during surgery better than the conventional method, according to the researchers.
These benefits allowed the operating surgeon to reduce the warm ischemic time for the 3D printing cohort by a statistically significant degree. The benefits also resulted in decreases in blood loss, surgical complications, and creatinine levels (a marker of kidney failure), compared with the conventional method, though the differences were not statistically significant.
The 3D printing technique proved to be even more advantageous for patients with a tumor of moderate to high complexity (a RENAL score of at least 8). In this subset of patients, 3D printing led to statistically significant reductions in warm ischemic time and intraoperative blood loss.
| Kidney cancer surgical planning with 3D printing vs. CT | ||
| Cases involving moderate to high tumor complexity | CT | 3D printing |
| Intraoperative blood loss* | 179.2 mL | 131.9 mL |
| Warm ischemic time* | 29.2 minutes | 24.6 minutes |
| Operating time | 168.4 minutes | 190.5 minutes |
| Overall complication rate | 13.8% | 8.7% |
The 3D printing technique was also associated with a decrease of five percentage points in the combined intra- and postoperative complication rate and a slight increase in operating time, although the differences were not statistically significant. Lowering the complication rate by roughly 40% highlights the potential for 3D printing to improve patient outcomes by enhancing surgical accuracy, the authors noted.
A conspicuous drawback of relying on the 3D-printed models, however, was that their production required patients to wait a longer period of time before receiving treatment. On average, the 3D printing patient cohort had to wait 6.6 more days before undergoing surgery, compared with the other patients. In addition, manufacturing the models cost approximately 3,200 yuan ($466 U.S.) per patient.
Nonetheless, using the 3D-printed kidneys did improve key measures of surgical quality, and the viability of integrating 3D printing into kidney-sparing surgery is likely to grow in light of anticipated cost-saving technological advancements in the near future, the authors concluded.