With a 1-tesla open scanner and some finesse, Chinese researchers are using MRI to guide percutaneous cryoablation of hepatic dome hepatocellular carcinomas (HCCs) to almost eliminate tumor progression and extend survival, according to a study published online March 12 in the American Journal of Roentgenology.
The researchers used MR fluoroscopy to acquire continuous images during the intervention, which they performed with a freehand surgical technique to confirm the entry point and route of the cryoablation needle. The group found that more than 94% of subjects reported no tumor progression, and only one patient died within one year following the procedure.
"The excellent resolution of MRI and freehand technique combined with MR fluoroscopy help to achieve the precise targeting of the cryoprobes," wrote the researchers led by Dr. Ligang Wang from the Affiliated Yantai Yuhuangding Hospital of Qingdao University. "The open scanner gives us abundant lateral space, which allows near real-time MR fluoroscopy in performing an interventional procedure."
HCC ranks as the third most deadly cancer worldwide. While surgical resection is often the optimum course of action, some debate remains about which imaging modality offers the best procedural guidance, especially since reaching lesions in the hepatic dome can be quite challenging.
Ultrasound-guided percutaneous cryoablation can be difficult due to overlapping images of the lung or ribs, and CT guidance involves an approach from below the diaphragm, which increases the risk of injury to or puncture of the lung. On the other hand, a 2016 study advocated the use of contrast-enhanced ultrasound to characterize tumors thought to be HCCs but that were indeterminate on MRI.
By comparison, MRI-guided percutaneous cryoablation has been used successfully to treat tumors in multiple organs with satisfactory results, the authors noted. MRI provides "excellent soft-tissue resolution and real multiplanar imaging capabilities, which are helpful to display and locate hepatic dome tumors more precisely than ultrasound and CT," they added.
To better determine the value of the MRI-guided procedure, the researchers sought to prospectively assess the feasibility, safety, and effectiveness of MRI-guided percutaneous cryoablation.
Wang and colleagues enrolled 37 consecutive patients (mean age, 57.2 years) with 37 HCCs located in the hepatic dome who underwent percutaneous cryoablation on a 1-tesla open MRI scanner (Panorama HFO, Philips Healthcare). An MR fluoroscopy T1-weighted gradient field-echo sequence was used to obtain images throughout the procedure, while clinicians employed a freehand technique to confirm the needle's entry and approach to the HCC.
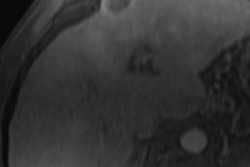
 Abdominal contrast-enhanced MR image acquired three months after cryoablation procedure. No enhancement surrounds the tumor ablation zone, and the ablation zone is diminishing in size. Image courtesy of AJR.
Abdominal contrast-enhanced MR image acquired three months after cryoablation procedure. No enhancement surrounds the tumor ablation zone, and the ablation zone is diminishing in size. Image courtesy of AJR.At the six-month follow-up, the researchers saw only one case (3%) of tumor progression, and all 37 patients (100%) were still alive. After one year, they saw two cases (5%) of tumor progression and one death, for a 12-month survival rate of 97%. The death was due to an upper gastrointestinal hemorrhage 10 months after cryoablation.
"Although the study was limited by the short follow-up and the number of patients, the outcome seems to be encouraging for the cryoablation of hepatic dome HCCs and comparable to the cryoablation and thermal ablation results in previous reports," Wang and colleagues wrote. "We think that these highly satisfactory results may be because of the precise navigation, precise guidance, and precise visualization of the ice ball in a 1-tesla open MRI system."