Radiologists using advanced visualization software to get the best coronary CT angiography (CTA) results might want to take another look -- once at the axial slices, that is, and once again using the software.
Radiologists in Germany and the U.S. have concluded that reading CTA data using advanced visualization techniques alone can miss many relevant stenoses that would have been found with a glance at the native CT data.
At the recent RSNA meeting in Chicago, Dr. Christopher Herzog from the University of Frankfurt in Germany talked about his group's pilot study comparing the use of advanced visualization tools alone to using them in combination with native CT images in coronary angiography.
"During the past several years, we have seen the rise of so-called advanced visualization tools," which are often the radiologist's only reading method for coronary CT angiography studies, Herzog said.
"VRT (virtual reality technology) or MIP (maximum intensity projection) displays are a very easy way to show the coronary arteries, and particularly interesting for arteries because it is the kind of visualization you don't have in angiography," he said. "The question is: Are they really good enough to just use them (alone), which was basically the aim of our study."
Herzog, along with his colleagues Drs. Peter Zwerner, Giancarlo Savino, and Thomas Vogl from the University of Frankfurt, and Dr. U. Joseph Schoepf from the Medical University of South Carolina in Charleston, examined 36 patients with suspected coronary artery disease.
All patients underwent both 64-detector-row CT angiography (Somatom Sensation, Siemens Medical Solutions, Erlangen Germany) of the coronary arteries and invasive coronary angiography.
The patients, most of whom were undergoing presurgical assessment prior to coronary artery bypass grafting (CABG) or stent implantation, were excluded for unstable angina, elevated creatinine (> 2.0 mg/dL) or allergy to iodine, but not for obesity or coronary artery calcification, Herzog noted.
The MDCT images were acquired with retrospective ECG gating after injection of beta blockers (5-15 mg intravenous metropolol for patients with heart rates faster than 65 bpm). The patients were given 0.4 mg nitroglycerine by mouth before scanning, and contrast media (50-75 mL Isovue [370 mgI/mL] Bracco, Milan, Italy) was injected using a bolus-triggering technique at 5 mL/sec, followed by a 50-mL saline chaser.
Images were acquired at 64 x 0.6 collimation using the z flying focal spot technique and retrospective ECG gating. Rotation time was 0.33 seconds, with pitch of 0.2, mAs of 120, and 900 kVp, Herzog said.
The readers were blinded to clinical data and angiography results. Beginning with the transverse images, they used standard 3D reformation techniques (MIP, multiplanar reconstruction [MPR]) either with or without the use of an advanced image visualization tool (AVT) (Circulation, Siemens).
Several weeks later the results of both methods were interpreted in combination, Herzog reported. Image quality (1-5) and extent of coronary artery disease (0-100% stenosis) were assessed on a per-segment basis. Interobserver variability was tested using Cohen's K test and CHI² contingency tables for level and significance. Spearman correlation was used to analyze the degree and correlation of the findings.
Angiography was performed using the Judkins technique. Three cardiologists with more than five years of experience each reviewed the data in consensus.
All CT coronary angiograms (36/36) yielded diagnostic-quality images, Herzog said. The mean image quality was good (4.1 ± 0.3), and 92.6% (500/540) of all segments were assessable without and 90.7% (490/540) with use of AVT respectively, Herzog reported.
The correlation coefficients for detection and grading of stenoses were r = 0.41 without use of advanced visualization techniques, r = 0.16 with use of AVT, and r = 0.64 for the combination of both (p < 0.05), the group reported.
Significant coronary artery disease, defined as stenosis of 50% or greater, was identified with 78.1% sensitivity (CI 46.3; 97.9%) and 90.9% specificity (CI 88.1%; 93.4%) without the use of advanced visualization techniques, with positive and negative predictive values of 41.6% and 94.9%, respectively.
With the Circulation advanced visualization software, CT angiography yielded 73.2% sensitivity (CI 57.7%; 85.4%) and 73.2% specificity (CI 65.6%; 73.4%), with positive and negative predictive values of 16.4% and 96.9%, respectively.
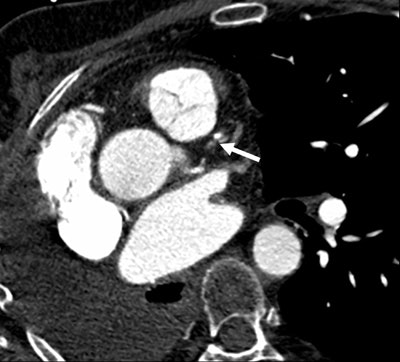 |
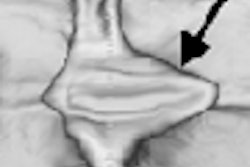
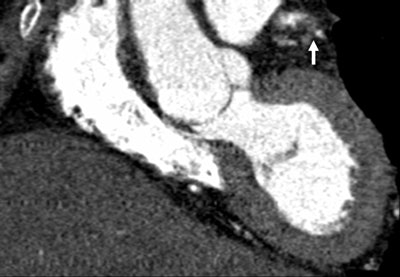
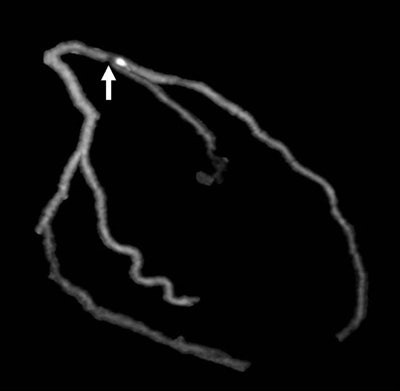
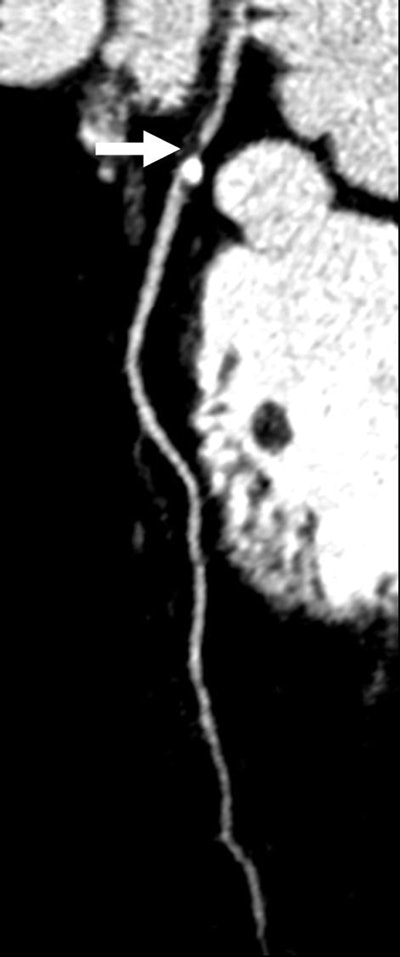
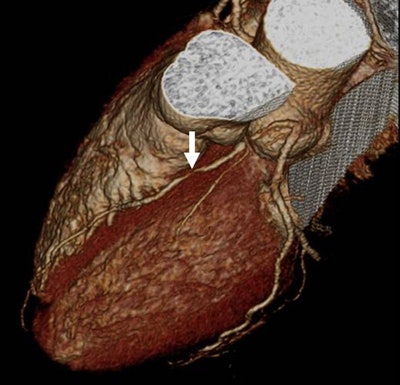
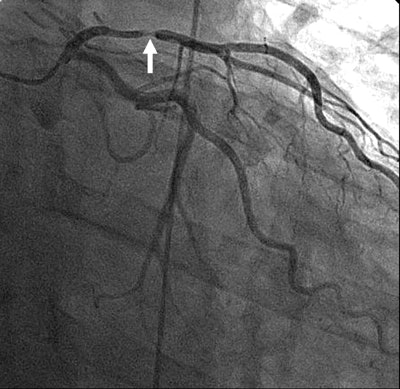
| Images 1-7 shown top to bottom: A 59-year-old man presented with atypical chest pain. A circumscribed, short-segment high-degree stenosis (arrow) in the proximal LAD is difficult to detect on transverse (1), sagittal (2), or coronal (3) multiplanar reformats. Use of advanced visualization tools with automated extraction of the coronary artery tree (4) and automated display as curved multiplanar reformat (5) clearly identifies the lesion, also seen in the 3D view (6) and confirmed on conventional catheter angiography (7). All images courtesy of Dr. U. Joseph Schoepf. |
 |
 |
 |
 |
 |
 |
The best results were seen when readers combined the two viewing methods. When advanced visualization techniques were used after previous visual assessment, the resulting sensitivity was 80.5% (95% CI 65.1%; 91.2%), with 96.2% specificity (95% CI 94.1% , 97.7%), positive predictive value of 63.5% (CI 48.9%; 76.4%), and a negative predictive value 98.4% (CI 96.8%; 99.3%). Thus, combining reading techniques yielded significantly (p < 0.05) better results than either method alone, Herzog said.
"It's important to say always look at axial slices, look for motion, look for misalignment of vessels," he said. "But if I limit myself to axial images, I invariably get into trouble as I move from the base to the apex."
The study showed that advanced image visualization tools are beneficial only if applied after previous visual inspection of the coronary arteries. A lot of radiologists confine themselves to advanced visualization reading methods, Herzog said, and they are doing themselves and their patients a disservice.
"Advanced visualization tools are not suitable as a standalone evaluation method for the detection and grading of coronary artery disease," he said. "However, if applied after previous visual inspection they help quantify the effective degree of stenosis, and thus significantly increase diagnostic accuracy."
By Eric Barnes
AuntMinnie.com staff writer
December 22, 2006
Related Reading
Cardiac CT yields significant extracardiac findings, November 26, 2006
Cardiac CT evolves on multiple fronts, November 20, 2006
CT pioneer test-drives 256-slice scanner, August 21, 2006
Study: 16-MDCT yields too many nonevaluable artery segments, July 26, 2006
Less radiation dose exposure in cardiac CT is possible, July 6, 2006
Dual-source imaging promises better CT scanning, June 15, 2006
Copyright © 2006 AuntMinnie.com