
A new algorithm called LevelCheck -- designed to prevent wrong-site spinal surgery -- boasted near-perfect accuracy in a trial by Johns Hopkins University researchers. By matching preoperative CT scans to intraoperative radiographs, LevelCheck confirms for surgeons that they are targeting the correct vertebral level.
Dr. Sheng-fu Lo and colleagues used LevelCheck to automatically label vertebrae in intraoperative mobile radiographs acquired during spine surgery in 20 retrospectively selected patients. The algorithm was 100% accurate when its full data-processing cycle was allowed to be completed, with accuracy dropping to about 99% when processing time was severely truncated to seven seconds.
"If you let it run for 25 seconds, it gets it right every time," said study co-author Jeffrey Siewerdsen, PhD, in an interview with AuntMinnie.com. "But 25 seconds is kind of a long time; it's OK but on the edge of what fits in the workflow."
Siewerdsen is a professor of biomedical engineering at Johns Hopkins University and an associate faculty member at the Armstrong Institute for Patient Safety and Quality.
First realistic test
Correct vertebral labeling is perhaps the most critical element in spine surgery, a setting where there is high potential for picking the wrong vertebral level based on visual impression, palpation, and fluoroscopy. The average wrong-surgery-site patient goes through significant pain and suffering, and the costs to fix the issue are substantial.
The incidence of wrong-surgery-site procedures is estimated to be one in every 3,110 spine surgeries, "implying that approximately 50% of spine surgeons will encounter a wrong-level error at least once in their career, with an approximate monetary cost of $127,000 per patient," the researchers wrote in the April 15 issue of Spine (Vol. 40:8, pp. E476-E483).
 Jeffrey Siewerdsen, PhD, from Johns Hopkins University.
Jeffrey Siewerdsen, PhD, from Johns Hopkins University.The LevelCheck algorithm is designed to automatically localize target vertebrae by registering preoperative 3D CT scans to 2D mobile x-ray images acquired in the operating room (OR). To localize spine levels, the process requires only that the target vertebra be labeled in the preoperative image -- for example, by pointing and clicking on a single vertebral area of interest. Then the same labels, in either their official anatomical names, such as T5 or T6, or in user-specific names such as "target," are placed on the corresponding spot on the radiograph.
The algorithm operates independently and finds the matching CT-imaged vertebra on the corresponding radiograph without the need for any specific tracking or navigation equipment.
Previously, the method was evaluated in 50,000 simulated trials (a trial being a single run of the software on an image dataset) with CT scans drawn from image archives of the U.S. National Cancer Institute. It showed registration accuracy of 0.2 ± 0.2 mm (mean and standard deviation of the projection distance error, or PDE) and a success rate (within 5 mm of the PDE) of 49,999 out of 50,000 patients.
A study on cadavers followed, using a wide variety of acquisition scenarios and deformations. In a total of 14,400 trials, LevelCheck yielded 99.99% accuracy, with a mean PDE of less than 1.0 mm and registration time of less than five seconds.
In the current study, the researchers wanted to investigate LevelCheck's performance under real-world conditions. They used the algorithm to examine images from 20 consecutive patients undergoing thoracolumbar spine surgery; all had received preoperative CT and intraoperative mobile radiography scans, which were examined retrospectively.
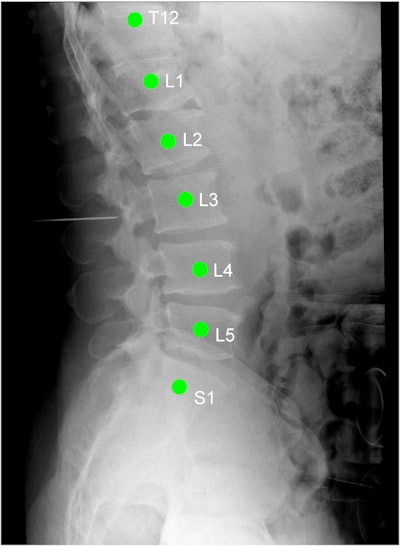 X-ray image of the thoracolumbar spine acquired during spinal surgery. The green labels are automatically applied by the LevelCheck algorithm as a decision-support aid and an independent check on target localization. Image courtesy of Jeffrey Siewerdsen, PhD.
X-ray image of the thoracolumbar spine acquired during spinal surgery. The green labels are automatically applied by the LevelCheck algorithm as a decision-support aid and an independent check on target localization. Image courtesy of Jeffrey Siewerdsen, PhD.The researchers examined 10,000 different views from those 20 patients to test the algorithm against the ground truth standard determined by the neuroradiologist. So many views were used because things aren't perfectly aligned in real clinical scenarios, Siewerdsen said. There may be different kinds of hardware involved, or perhaps the technologist made the field-of-view very small to save dose.
"If you have the image perfectly aligned to start with, it's going to be able to automatically get it right," Siewerdsen said. "But we said, let's perturb that initial estimate between CT and the radiograph and what we think the pose of that radiograph is, and make it crooked 1,200 different times with varying degrees of severity in that perturbation, and then see if the algorithm can wrestle it back and render the vertebrae accurately."
To assess trade-offs between registration accuracy and computation time, each trial or simulation was registered with parameter settings of variable multistarts, a measure of the number of computation steps used during localization. The more multistarts, the more robustness against anatomical deformation.
The computation time for 50, 100, 150, and 200 multistarts was 7.1, 13.1, 17.8, and 25.7 seconds on a 2.4-GHz desktop PC. The LevelCheck algorithm labeled the intraoperative mobile radiograph spinal levels (mPDE < 5 mm) and calculated them as a function of the number of multistarts and computation times, the authors explained.
At a computation time of about 26 seconds, the registration accuracy was 100% across all 10,000 trials. As the computation time and the number of multistarts decreased, the registration remained fairly robust, down to 99.3% registration accuracy at seven seconds:
- 100% at 26 seconds (200 multistarts)
- 99.97% at 18 seconds (150 multistarts)
- 99.86% at 13 seconds (100 multistarts)
- 99.3% at seven seconds (50 multistarts)
No differences were found in the rate of successful registration between the 13 patients undergoing primary operations and the seven undergoing revision surgery. Failure modes were analyzed for any trial yielding mPDE of more than 5 mm -- these totaled 70 of the 10,000 trials, at the truncated run time of seven seconds.
The researchers noted an in-plane error resulting in a registration shift of an entire vertebral body, as well as an out-of-plane error causing the registration to be inaccurate but not off by a full vertebral body level.
"The LevelCheck algorithm correctly identified target vertebrae in intraoperative mobile radiographs of the thoracolumbar spine, demonstrating acceptable computation time, compatibility with routinely obtained preoperative CT scans, and warranting investigation in prospective studies," the study team concluded.
The method offers great potential as a decision-support tool and an independent check against wrong-level surgery, with clinical studies now underway, the authors wrote.
"We're doing a larger retrospective study of 500 cases," and under a U.S. National Institutes of Health (NIH) grant, "we're doing a prospective study in the OR under research protocols, again to test practicality and feasibility in the OR," Siewerdsen said.
The plan is that surgeons would continue to use the current technique of level counting. Then, after they've completed their localization, the investigators would ask them if the method would have helped in their decision-making, and whether they would have reached the same result without it.



















