Automated 3D segmentation software can help radiologists identify pulmonary hypertension on CT pulmonary angiography (CTPA) exams, according to research published online April 28 in the American Journal of Roentgenology.
Researchers from Heidelberg University Hospital in Heidelberg, Germany found that automated volumetry of the cardiac chambers -- particularly of the right atrium -- on nongated CTPA exams offered incremental utility over conventional parameters on echocardiography as well as CTPA exams for diagnosing pulmonary hypertension. What's more, a predictive model that incorporated both CTPA and echocardiographic analysis together yielded an area under the curve (AUC) of 0.898.
"Automated volumetry of cardiac chambers based on nongated CTPA may facilitate early noninvasive detection of [pulmonary hypertension], identifying patients who warrant further evaluation by [right heart catheterization]," wrote first author Dr. Claudius Melzig and colleagues.
Although early diagnosis of pulmonary hypertension is crucial to prevent chronic progression and a poor prognosis, the condition's nonspecific symptoms may contribute to a delay in diagnosis. As a result, noninvasive tests are needed to help select patients for diagnostic right heart catheterization, according to the authors.
In their study, the researchers sought to investigate the potential benefit of cardiac chamber volumetry on nongated CTPA exams, which are commonly performed in patients with suspected pulmonary hypertension. They retrospectively assessed 109 patients from August 2013 to February 2016 who had received CTPA, echocardiography, and right heart catheterization. Of these patients, 60 were found after right heart catheterization to have pulmonary hypertension and 49 did not.
Two radiologists with one and three years of cardiovascular imaging experience independently reviewed the exams, blinded to clinical data and measurements from any other imaging examinations. They used version 11 of the IntelliSpace Portal software (Philips Healthcare) to perform automated 3D segmentation of the right ventricle, left ventricle, right atrium, and left atrium on CTPA.
After viewing the automated segmentation results, the radiologists manually corrected visible deviations from the chamber contours using the software's brush tools. They also measured the diameters of all cardiac chambers, the main pulmonary artery, and the ascending aorta.
One of the radiologists reevaluated half of the cases a year later to assess intraobserver variability. Overall, the automated volumetry method yielded excellent intraobserver and interobserver agreement for the various measurements; intraclass correlation coefficients (ICC) ranged from 0.935 to 0.999 for intraobserver agreement and ICCs ranging from 0.830 to 0.978 for interobserver agreement.
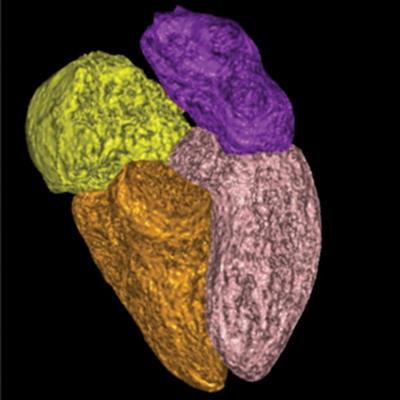
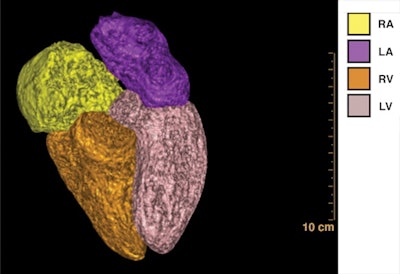 3D visualizations of cardiac chamber based on segmentation of chambers on CT pulmonary angiography (CTPA) in a 57-year-old woman with pulmonary hypertension. CTPA image shows enlargement of right heart, particularly of right atrium. RA = right atrium, LA = left atrium, RV = right ventricle, LV = left ventricle. Image and caption courtesy of the American Journal of Roentgenology.
3D visualizations of cardiac chamber based on segmentation of chambers on CT pulmonary angiography (CTPA) in a 57-year-old woman with pulmonary hypertension. CTPA image shows enlargement of right heart, particularly of right atrium. RA = right atrium, LA = left atrium, RV = right ventricle, LV = left ventricle. Image and caption courtesy of the American Journal of Roentgenology.After adjusting for age, sex, and body surface area, the researchers found that four variables were significant predictors of pulmonary hypertension -- as defined under the 2018 hemodynamic definition from the Sixth World Symposium on Pulmonary Hypertension. These included the following:
- Right atrial/left atrial volume ratio (odds ratio, 11.22)
- Right atrial/left ventricular volume ratio (odds ratio, 2.91)
- Right atrial volume per 10 mL (odds ratio, 1.27)
- Right ventricular volume per 10 mL (odds ratio, 1.21).
After performing regression analysis, the researchers developed a predictive model that yielded excellent diagnostic performance based on just two significant predictors -- pulmonary artery systolic pressure on echocardiography and right atrial volume.
| Performance of predictive model combining CTPA and echocardiography | |
| AUC | 0.898 |
| Sensitivity | 83.3% |
| Specificity | 85.7% |
"The findings indicate a role for automated 3D volumetry of cardiac chambers based on nongated CTPA, to be used in conjunction with transthoracic echocardiography for the early noninvasive detection of [pulmonary hypertension], in possibly identifying patients for whom further evaluation by [right heart catheterization] is warranted," the authors wrote.




















