A nomogram based on MRI radiomics can help clinicians predict if individuals with osteoarthritis will experience an improvement in knee pain over a two-year course of taking oral vitamin D supplements, according to research published on November 2 in Osteoarthritis and Cartilage.
The results address the often tricky problem of how to best evaluate and manage osteoarthritis, according to a team led by Dr. Ting Lin of Southern Medical University in Guangzhou, China.
"The most important hurdle in osteoarthritis management is the lack of provision of a simple and quantitative biomarker that can provide breakthroughs in clinical management," the authors noted. "Our study constructed the radiomics signature as a useful biomarker that showed favorable predictive performance."
One way researchers have explored mitigating osteoarthritis joint pain is through patients' use of vitamin D. But studies on this tactic have produced mixed results, with some finding that the vitamin doesn't help and others finding that it can be useful in about a third of those with osteoarthritis.
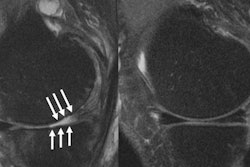
How can clinicians predict whether vitamin D therapy will work? Lin's team hypothesized that an MRI radiomics-based nomogram could help. They selected MRI because it is noninvasive and measures structural abnormalities that may then be used as biomarkers that indicate osteoarthritis progression.
The research included data from 216 people who participated in the Vitamin D Effects on Osteoarthritis (VIDEO) study for which the primary outcome was a 20% improvement in knee pain score after two years of either taking vitamin D supplements or a placebo.
Lin's group extracted radiomics features of MRI exams of the subchondral bone and incorporated clinical characteristics (i.e., gender, baseline knee pain score, vitamin D intervention, muscle strength, area of cartilage damage) from patients with knee pain, randomizing the data into training and validation sets to create the radiomics model. They then used the model to develop a nomogram for predicting osteoarthritis knee pain improvement over two years.
Except for female sex and baseline knee pain score, adding clinical characteristics to the nomogram did not produce statistically significant differences in its ability to predict pain improvement. But the MRI radiomics data did.
| Predictive performance of clinical model and MRI radiomics-based nomogram on validation data | ||
| Clinical model | MRI radiomics-based nomogram | |
| Area under the curve (AUC) | 0.71 | 0.83 |
| Sensitivity | 88% | 76% |
| Specificity | 47% | 84% |
"[The nomogram] could help clinicians improve patient-physician communication, decision making, and even to choose suitable patients for a certain treatment in advance," the authors concluded. "This proof-of-concept study could facilitate individualized medicine."