An artificial intelligence (AI) algorithm can identify racial or ethnic health disparities in COVID-19 patients based on the analysis of chest radiographs, according to research presented Wednesday at RSNA 2021 in Chicago.
A research team led by presenter Dr. Ayis Pyrros of Duly Health and Care in Chicago developed a deep-learning model that yielded highly accurate assessments of comorbidities in COVID-19 patients. What's more, it yielded comorbidity scores that were predictive of a patient's self-reported race.
"Unequal burden of comorbidities is a primary contributor to health disparities, and [deep-learning] modelling can predict these relevant comorbidities among COVID patients, helping to identify those who may benefit from mitigation," Pyrros said.
In an effort to detect health disparities among COVID-19 patients, the researchers sought to develop a deep-learning model to predict Medicare Advantage Hierarchical Condition Category (HCC)-related comorbidities, according to Pyrros.
"This is important because racial/ethnic minority populations tend to have a greater burden of underlying comorbidities [that] can increase the risk of mortality from COVID-19," Pyrros said. "It has been reported that non-white patients hospitalized with COVID were more likely to have a higher severity infection associated with limited English proficiency."
HCC codes are groupings of ICD-10 codes that are tied to value-based payments. However, health disparities are hard to detect at the individual patient level, Pyrros said.
"We have a very fragmented U.S. healthcare system," he said. "The absence of a diagnosis code in itself is a health disparity. These codes are actually predictive of mortality in COVID-19."
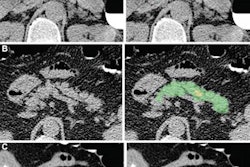
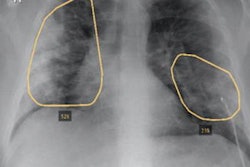
As a result, the researchers sought to utilize a "neural network to connect the codes to the x-ray and convert the images into biomarkers of patients' chronic disease burden," Pyrros said.
Using over 14,000 ambulatory frontal chest x-rays, the multi-institutional team of researchers trained a multitask deep-learning model to predict comorbidities and then associate these findings with self-reported race/ethnicity recorded in the electronic health record (EHR) software.
In testing on 814 COVID-19 patients, the algorithm yielded an area under the curve (AUC) of 0.99 for predicting patient sex, 0.91 for morbid obesity, 0.88 for congestive heart failure, 0.87 for vascular disease, 0.81 for cardiac arrhythmias, and 0.80 for predicting diabetes with chronic complications.
When modeled with logistic regression analysis, the algorithm's comorbidity scores for chronic obstructive pulmonary disease (COPD) and cardiac arrhythmias were significantly associated with self-reported race/ethnicity (p < 0.05). Overall, the deep learning-based comorbidity model yielded an AUC of 0.65 for predicting self-reported race, compared with 0.61 when using the Medicare Advantage HCC Risk Adjustment Model calculated from EHR data.
"A multiclass deep-learning algorithm using only a frontal chest radiograph was predictive of select comorbidities," he said. "And the comorbidity scores modeled with logistic regression were predictive of self-reported race and ethnicity, with significant differences from EHR data."
Pyrros noted, though, that "you don't need AI to report on cardiomegaly, COPD or atherosclerosis," he said. "Sometimes [these] things get lost, and this is something you can do every day and actually eventually help a patient."