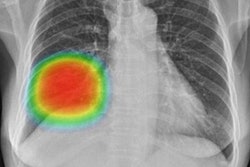
New research from South Korea shows that in countries using x-ray as part of population health check-ups, artificial intelligence (AI)-based software may improve the detection of lung nodules, according to research presented at the recent RSNA meeting in Chicago.
Studies have suggested that AI-based computer aided detection (CAD) for chest x-ray performs equal to or better than radiologists and improves radiologists' interpretations when used as a second reader. But these studies have often been conducted using datasets collected retrospectively, arbitrarily selected and often of disease-rich and dichotomized composition, yielding consequent selection bias, noted Dr. Ju Gang Nam, a radiologist at Seoul National University Hospital (SNUH). Reader performance tests are also conducted retrospectively with similar performance bias, and proper integration of AI-CAD with conventional PACS is often lacking, according to Nam.
"We aimed to investigate if a commercial AI-based software may increase the detection rate of clinically significant, actionable lung nodules on chest x-rays in a health check-up population through a randomized, controlled trial. In addition, for this prospective trial we integrated AI-CAD into a commercial PACS (AI-PACS) and incorporated it into the real clinical work process," Nam told attendees at the meeting. "AI-based software enhanced detection of clinically significant lung nodules on chest x-rays without increasing false referral rate."
In this single-center, double-arm, open-label clinical trial, 11,062 x-rays were taken from 10,476 individuals in SNUH's healthcare screening center. Subjects were all adults over the age of 18 who visited the health screening center for a chest x-ray exam.
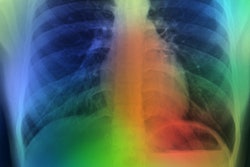
After x-ray acquisition, images were sent to the AI-CAD (Lunit INSIGHT CXR version 2.0.2.0) server and the AI-PACS (Infinitt Healthcare) server simultaneously, with the AI-PACS server randomizing patients 1:1 to one of the two groups; the experimental arm (AI-group; subject n = 5238, x-ray n = 5549) or the control arm (non-AI group; subject n = 5,238, x-ray n = 5,513).
One of three designated radiologists interpreted each x-ray using a structured reporting format integrated in AI-PACS and referring to the AI-CAD software results for subjects in the AI group.
Primary outcome was the detection rate of clinically significant lung nodules confirmed on CT taken within three months, where significant nodules were defined as solid nodules larger than 8 mm or subsolid nodules with a solid portion larger than 6 mm (Lung-RADS category 4). Pathologic results were reviewed four months after trial termination. Detection rate was defined as the number of true-positive x-rays divided by the total number of x-rays. Secondary outcomes included positive rate, sensitivity, false referral rate, and lung cancer detection rate.
The researchers compared primary and secondary outcomes between the two groups. Subgroup analyses were also performed using demographics, medical history, and radiologist readers.
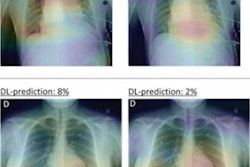
The trial demonstrated an increased detection rate of Lung-RADS category 4 nodules in the AI-group (AI vs. non-AI-group; 0.59% [31/5,238] vs. 0.25% [13/5,238]; p = 0.008).
Chest CT was obtained between the two groups within three months. Among those who underwent chest CT, the prevalence of significant nodules was similar and the performance of chest x-ray showed increased sensitivity in the AI group. Chest x-ray for these AI group patients also showed higher positive and negative predictive values, with very few false positives.
There was no difference in positive rates on x-rays and false referral rates. Twenty-four individuals were diagnosed with primary lung cancer (16 in the AI group and 8 in the non-AI group) and there was no significant difference in lung cancer detection rates.