A deep-learning model based on mammographic images can determine tumor staging and sentinel lymph node metastasis in breast cancer patients, a study published April 15 in Informatics in Medicine Unlocked found.
A team led by Elaheh Tarighati Sereshkeh from the Iran University of Medical Sciences in Tehran found that its convolutional neural network (CNN) model achieved high performance marks in these areas.
“This method can be used as a potential non-invasive tool to determine tumor staging and sentinel lymph node metastasis in breast cancer in people suspected of having the complication and to avoid unnecessary surgery,” Sereshkeh and colleagues wrote.
CNNs have been used in AI research to classify breast cancer disease status and predict therapeutic responses based on diagnostic images of the primary breast tumor. The researchers highlighted that CNNs require little preprocessing compared with other image classification algorithms. While such diagnosis technology can be used to help doctors diagnose breast cancer, the researchers also emphasized that “there is still much to be improved.”
Sereshkeh's group explored the potential of a CNN-based deep learning model that incorporates deep features resulting from mammography staging. The team suggested that such modeling can help determine tumor staging and lymph nodes before surgery in breast cancer patients.
The study included a retrospective dataset of 390 breast cancer patients. For their model, the researchers collected pathological variables from medical records. These included the following age, tumor location, staging based on the American Joint Committee on Cancer (AJCC), pathological type, human epidermal growth factor receptor 2 (HER2) status, progesterone receptor (PR) status, and estrogen receptor (ER) status.
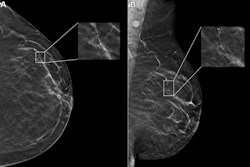
The authors also applied a contrast enhancement technique with Contrast-Limited Adaptive Histogram Equalization (CLAHE) to the studied data using MATLAB software. The images were first changed from color to gray in the preprocessing process, and then the images were changed from gray to color again. Finally, two expert radiologists isolated the regions of interest of the primary tumor from other areas of breast tissue.
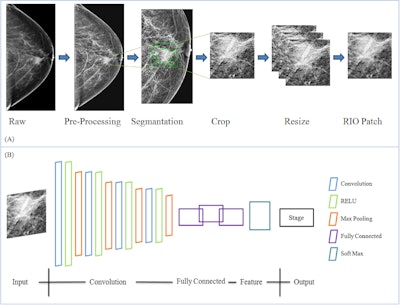 Researchers explain the data preparation and structure of a proposed CNN-based deep learning model using mammography features to determine breast tumor staging. The image is available for use under a Creative Commons license: CC BY-NC-ND 4.0 DEED Attribution-NonCommercial-NoDerivs 4.0 International.
Researchers explain the data preparation and structure of a proposed CNN-based deep learning model using mammography features to determine breast tumor staging. The image is available for use under a Creative Commons license: CC BY-NC-ND 4.0 DEED Attribution-NonCommercial-NoDerivs 4.0 International.
From each patient, the model extracted 4,096 features from mammograms and selected six related features according to the relationship between tumor size determination and lymph node metastasis.
Out of the total women included in the study, 300 had metastatic sentinel lymph node involvement and all women had a tumor size greater than 1 mm. Also, 273 of the women were placed into a training cohort while 117 were placed into a validation cohort.
The CNN-based model achieved an area under the receiver operating curve (AUC) of 0.919 for the training group and an AUC of 0.877 for the validation group. This included accuracies of 0.796 and 0.758, respectively.
The study authors highlighted that using data from preoperative mammography images can help assess tumor characteristics and clinical staging and treatment strategies.
“Also, [with] the ease of access and cheapness and diagnosis of the gold standard of breast cancer, mammography in the diagnosis and evaluation of breast tissue diseases has been more appropriate than ultrasound and MRI imaging,” they added.
They also wrote that appropriate treatment planning for early diagnosis and treatment can reduce cost and increase patient survival.
The full study can be found here.