An AI-based method can outperform models based just on breast density analysis for identifying patients who would benefit from supplemental imaging, according to research published April 9 in Radiology.
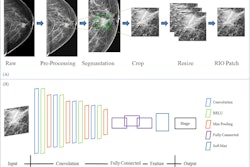
A team of researchers from Sweden led by Yue Liu of KTH Royal Institute of Technology in Stockholm developed AISmartDensity, an AI-based score that incorporates results from three algorithms for analyzing cancer signs, masking, and risk. In testing, the score outperformed traditional mammographic density measurements in flagging patients for supplemental breast imaging following a negative screening mammogram.
What’s more, the AI score could potentially have saved more than twice the number of years of life than relying on density measurements.
“In clinical practice, individuals with very high AISmartDensity score may benefit from supplemental screening tests to enhance early detection,” the authors wrote. “Moreover, this risk categorization might also prompt an additional image review by radiologists, particularly when informed of a high AISmartDensity score.”
To see if AI could improve breast density measurements, the researchers performed a retrospective study involving 65,235 mammographic examinations – 64,870 normal exams and 455 in cancer patients – that were bootstrapped from 2,043 patients receiving screening mammograms at Karolinska University Hospital between January 2008 and December 2015. They compared the performance of AISmartDensity with mammographic density percent and dense area, as well as age-adjusted versions of these measures.
| Performance for identifying future breast cancers | ||
|---|---|---|
| Best-performing density model | AISmartDensity score | |
| Identifying future cancers within 3 years | 57 of 455 (13%) | 152 of 455 (33%) |
| Positive predictive value | 1.09% | 2.91% |
| AUC | 0.61 | 0.72 |
| Identified interval cancers | 21 of 130 (16%) | 41 of 130 (32%) |
| Identified next screening-round detected cancers | 30 of 325 (9%) | 111 of 325 (34%) |
What’s more, the AI score could have potentially saved 1,579 years of life, more than twice the estimated 675 years saved with the best-performing density measure, according to the researchers. All differences were statistically significant.
“In conclusion, AISmartDensity effectively identified patients who were likely to benefit from supplemental imaging after a negative screening mammogram,” they wrote.
The researchers noted that their model is currently acting as a postscreening reader in a randomized clinical trial to flag high-risk mammograms for supplemental MRI. This trial will provide further evidence of the model’s real-world performance in a clinical setting, according to the authors.
“This study highlights the potential of AI-based risk prediction in the era of personalized screening, offering precise identification of individuals who could benefit from supplemental imaging, which is a step towards customizing screening protocols and optimizing screening initiation and frequency,” wrote Myoung Kyoung Kim, MD, of Sungkyunkwan University School of Medicine and Jung Min Chang, MD, of Seoul National University College of Medicine, in an accompanying editorial.
The full article can be found here and the editorial can be found here.