The radiology department at the Mayo Clinic in Rochester, MN, has developed database software to capture adverse events and patient safety-related issues. The program has evolved into an extremely valuable quality assurance tool for the department.
The internally developed Web-based software took three years to perfect, but it's attributed with uncovering safety gaps for which prospective corrective processes and procedures were developed. It has improved communication within the department, in addition to facilitating a culture change in operations, according to an article in the September issue of the American Journal of Roentgenology.
In 2004, the radiology department developed an interdepartmental reporting system to capture safety events and concerns, as well as environmental hazards and process flaws. It was intended to provide a consolidated means of recording and analyzing safety issues and more rapidly facilitating interventions. However, the system was paper-based, unwieldy, and difficult to use.
It was replaced in 2005 by a database software system that categorized 10 event types and had its own desktop icon for easy access. Department staff members were encouraged to report near misses and "good catches" so that processes could be improved. However, the system was not as efficient as it could be because it required handwritten event reports to be entered manually (AJR, September 2011, Vol. 197:3, pp. 684-688).
In 2007, the system was replaced with Web-based software. It eliminated the paper form and prepopulated several data-entry fields (e.g., when a medical record number was added, patient information fields were prepopulated). Forced-entry fields -- including event date, type, description, location, and modality involved -- prevented incomplete forms from being submitted. Reports could be efficiently and rapidly sent to division directors within the department, and data retrieval was simplified with a search capability.
Additional enhancements were also added, such as help functionality, training videos, pop-up screens, and supplemental data-entry fields. A field was added indicating whether the event necessitated calling the hospital's sentinel event team. As the utility of the system improved along with ease of use, so did the number of users reporting events, and first-line managers began to use the data to initiate quality improvement projects.
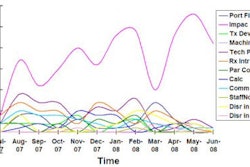
In calendar year 2005, only 325 events were reported. This steadily increased to 1,116 in 2009. During this time period, the department performed an average of 930,000 exams per year.
Most submissions were made by radiologic technologists (43%) and nurses (36%) and related to high-throughput modalities: general radiology (32%), CT (30%), MRI (13%), and ultrasound (13%). Inappropriate exams and patient identification issues represented the highest categories reported.
Many quality improvement initiatives have been undertaken as a result of the radiology event reporting system, lead author Dr. Stacy Schultz and colleagues wrote. These include changes in reporting semiurgent findings, reviewing radiology orders, and implementing computerized physician order entry (CPOE).
Other changes involved improving the detection of ferromagnetic objects in MRI suites, changing processes relating to patients who require oxygen, and reducing inefficiencies involving peripherally inserted central venous catheter lines.
Communication also improved, with section supervisors receiving monthly reports that are discussed at operational group meetings. The reporting system permits a more proactive approach, benefiting both patients and department operations alike.