A combination of clinical decision-support software and a good rapport between emergency physicians and radiologists is credited for decreasing the number of CT pulmonary angiography (CTPA) exams ordered to evaluate acute pulmonary embolism (PE).
Brigham and Women's Hospital in Boston, which sees 60,000 emergency department admissions each year, was able to reduce the number of exams ordered by 20% and increase its yield by nearly 70%, according to an article published online December 20 in Radiology.
During a five-year period before Brigham and Women's implemented an evidence-based clinical decision-support system interfaced with its computerized physician order-entry system (CPOE), it had experienced an 82.1% increase in the ordering of CTPA exams by emergency physicians. In August 2007, a clinical decision-support system (Percipio, Medicalis) was implemented in the emergency department.
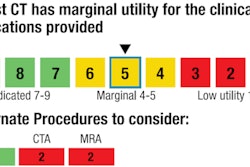
When an emergency physician placed an order for a CTPA exam to confirm or rule out acute PE, three consecutively displayed screens were activated. The first required the ordering physician to indicate the level of suspicion of PE and complete a D-dimer level assessment. If a D-dimer assay had not been performed and the level of suspicion was low or intermediate, another window suggested that the D-dimer assay should be performed before ordering the CT exam.
If the D-dimer assay had been performed and was normal and the physician had selected a low or intermediate level of PE suspicion, the system recommended that the CT exam not be ordered.
Physicians could cancel their order after each screen display, or they could continue with the order. However, the researchers found that the emergency department physicians began to heed the advice that the procedure might be unnecessary.
Lead author Dr. Ali Raja, an emergency physician, and colleagues analyzed data from October 2003 through September 2009 to determine the impact of the clinical decision-support software. A database search indicated that a total of 6,838 patients out of more than 3.3 million patients admitted had undergone a CT pulmonary angiography exam, approximately 2% of the total. Before implementation, from October 2003 through July 2007, the number of exams increased from 14.5 to 26.4 patients per 1,000. Starting August 2007, this dropped each consecutive quarter, to 21.1 patients per 1,000 by September 30, 2009.
The authors attribute this achievement to several factors:
- The clinical decision-support software focused on a specific clinical indication and specific diagnostic modality, which they felt increased acceptance of the recommendations.
- The software rollout was supported by champions in the emergency department, an education campaign, and interdepartmental meetings to discuss it.
- A proactive quality improvement initiative was under way in the hospital, and there was also a heightened awareness about minimizing patients' radiation dose exposure.
Raja and colleagues identified three characteristics that differentiated the patients suspected of having acute PE who underwent the CT exam from those who did not. These patients were more likely to have had a history of thromboembolism and less likely to have had recent surgery or D-dimer testing. On average, the number of D-dimer tests decreased by 10% after implementation, a factor attributed to the presumption that the software identified higher risk patients who needed the CTPA exam.