
VIENNA - Harder, better, faster, stronger: It's not just a song, it could also be the mantra for radiologists as they try to improve workflow efficiency and quality. This morning's computer applications refresher course covers radiology reports and dose management, plus computerized order entry. Enhancing radiology reports and becoming more familiar with dose management regulations and registries can help in this process.
When it comes to reporting, there are two types of structures: clinical and technical. Clinical structure is important because it conveys information to someone else about a patient. Technical structure is important because it allows for the easy (or sometimes not so easy) transfer of images and reports from one institution to another.
 Dr. Neelam Dugar is a consultant radiologist at Doncaster Royal Infirmary, U.K., and former chair of the Royal College of Radiologists' Imaging Informatics Group.
Dr. Neelam Dugar is a consultant radiologist at Doncaster Royal Infirmary, U.K., and former chair of the Royal College of Radiologists' Imaging Informatics Group.
"In radiology, we can't give normal or abnormal reports -- these are complex tests," said Dr. Neelam Dugar, consultant radiologist at Doncaster Royal Infirmary, U.K., and former chair of the U.K. Royal College of Radiologists' Imaging Informatics Group, in an interview with ECR Today. "We're like the conductor of the orchestra. I like that analogy because we're hugely involved and giving a direction to the way the patient needs to be managed."
Dugar structures clinical reports to include the indication (why the test is being done), findings, description, conclusions, and recommendations. Radiologists don't create reports for themselves, they create reports to communicate, which is why the format, structure, narrative content, and technical aspects need to be clear and easy to follow, she added.
"There have been lots of talks about structured reports," she said. "Often the previous talks have been about how we can structure the narrative content into drop-down menus, which is not possible for complex imaging. Radiology reports are opinion. ... Disease doesn't follow the rules, and that's why you can't have computers diagnosing patients."
Much of the complexity lies in the technical structure. While it sounds like it would be an easy task to send images and reports somewhere else, it can be quite troublesome. It's fairly easy to transfer images because of DICOM standards, but trying to transfer reports from one place to another may be difficult, Dugar said.
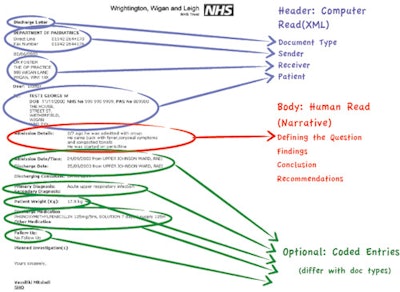 This figure shows an example of a clinical document architecture discharge letter. The same principles apply for a radiology report: namely, ease of conveying information. Image courtesy of Dr. Neelam Dugar.
This figure shows an example of a clinical document architecture discharge letter. The same principles apply for a radiology report: namely, ease of conveying information. Image courtesy of Dr. Neelam Dugar."We have suddenly ended up with very bad practices that are going forward to PACS," she remarked. "The worst practice we've ended up with is ordering reports and images in an electronic world. That is causing enormous problems. Radiologists would have had the request, they would have looked at it in a proper light, and suddenly those images go off to somewhere else."
For instance, a radiologist in another hospital may be asked by someone to take a look at the images. The individual has no prior knowledge of what has gone on and there is a danger of giving an inaccurate, incomplete report. Because there is no report, a radiologist has to generate a new one and time has been wasted, Dugar explained.
It's important to bring together both sides of structured reporting, and from a clinical perspective, we need to indicate what we want from structured reports, she noted. In her lecture, she also focuses on the IT aspects of the entire process.
Another problem area is radiation dose. Eliseo Vaño, PhD, professor of medical physics in the radiology department of Complutense University in Madrid and at the San Carlos University Hospital, is focusing on this area during today's session.
 Radiologists must learn about dosimetry so they can estimate radiation dose and justify an imaging procedure. Here, radiologists perform a cardiovascular procedure at San Carlos Hospital. Image courtesy of Eliseo Vaño, PhD.
Radiologists must learn about dosimetry so they can estimate radiation dose and justify an imaging procedure. Here, radiologists perform a cardiovascular procedure at San Carlos Hospital. Image courtesy of Eliseo Vaño, PhD.
The European directive on medical exposure requires patient radiation doses to be assessed and evaluated, especially in procedures involving high doses to the patient. In the current draft of the new directive of "Basic Safety Standards," some requirements on patient dosimetry have been reinforced, and x-ray systems are expected to provide dosimetric information with the capacity to transfer the information to the exam report for all CT and interventional systems, he said.
Patient dose limits do not apply, but diagnostic reference levels (DRLs) will be used to help optimize clinical procedures. The new European directive will require a periodic update when new technology can allow patient radiation dose reduction while maintaining enough image quality, Vaño added.
"These requirements will push the industry and the users to develop better strategies to evaluate patient doses, to transfer these values to the patient reports -- contributing to the patient dose tracking system -- but also to offer software to process these dosimetric data and to do some automatic analysis," he said.
Radiologists need to learn about dosimetry because the knowledge of patient doses and the estimation of radiation risk is a key point when justifying some imaging procedures and is helpful when selecting the most appropriate imaging modality, he noted. Radiologists and radiographers have to optimize the procedure, or use the appropriate protocols to obtain the necessary diagnostic information with the lowest radiation dose compatible with the needed image quality.
 Radiation protection for patients and workers is taken seriously at this cath lab at San Carlos Hospital in Madrid. Image courtesy of Eliseo Vaño, PhD.
Radiation protection for patients and workers is taken seriously at this cath lab at San Carlos Hospital in Madrid. Image courtesy of Eliseo Vaño, PhD.
Vaño's talk covers aspects of the existing and future European regulations on radiation safety for patients and the advances in technology to allow the measurement, transfer, recording, and analysis of patient doses in imaging procedures as well as the comparison with DRLs in quality programs.
"Radiologists should know some basic aspects of radiation doses and radiation protection as part of the quality culture and to avoid any unnecessary increase of radiation risk to the population," he concluded.
Originally published in ECR Today on 11 March 2013.
Copyright © 2013 European Society of Radiology



















