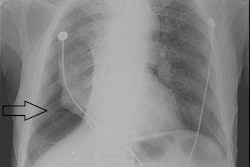
Radiography has played a key role in managing the COVID-19 pandemic. Radiologists on the front lines of the outbreak have found chest x-ray to be a useful complement to other tools for diagnosing patients with COVID-19 and tracking their prognosis.
Among x-ray's advantages are its low cost and versatility, especially in an environment dominated by concerns about infection control. The important issue when using x-ray for COVID-19 is to know the limitations of the modality when making a diagnosis.
Radiography can complement other tools, like CT, lung ultrasound, and reverse transcription polymerase chain reaction (RT-PCR) tests, to help clinicians make a diagnosis of COVID-19. And x-ray's value is for more than just diagnosis -- it is also invaluable as a prognostic tool that can help predict the likely course of COVID-19.
While radiography may not have the greatest diagnostic power, it still can play a key role in managing the COVID-19 pandemic.
Pros and cons
Compared with CT, radiography is inexpensive and readily available. While its 2D images may lack the detail of CT, it delivers far less radiation dose.
What's more, mobile x-ray enables imaging to be taken to the patient's bedside, which confers huge advantages for COVID-19 detection. This keeps infected patients out of a hospital's radiology department and avoids the need to sanitize radiology rooms after use.
Recent research is showing that x-ray can help in the COVID-19 battle. Chest x-rays acquired when patients present in the emergency room (ER) with COVID-19 symptoms can help predict the severity of the disease, particularly in young and middle-aged adults, according to a study published May 14 in Radiology. The study findings demonstrate x-ray's value in helping physicians identify, triage, and treat high-risk patients, wrote a team led by Dr. Danielle Toussie of Mount Sinai Hospital in New York City.
"Our study demonstrated that the initial portable chest x-ray obtained in the emergency department of patients with suspected or known COVID-19 can predict key clinical outcomes, including the need for hospitalization or need for intubation," Toussie told AuntMinnie.com. "It is not necessarily the x-ray that is used for diagnosis, but rather for prognosis."
In fact, with more RT-PCR testing available, x-ray's utility is even higher as a prognostic tool, especially since CT shouldn't be used widely, Toussie said.
"Our study showed that the simple portable single frontal-view chest x-ray is actually sufficient to provide invaluable information on how the patient may portend once they have a diagnosis of COVID-19," she explained.
Other studies have validated Toussie's research for all age groups. Investigators at IRCCS San Raffaele Hospital in Milan, Italy, reported in a letter in Radiology how they used a severity score to retrospectively assess the prognostic value of chest x-ray performed upon initial presentation of 246 patients who had their COVID-19 diagnosis confirmed by RT-PCR.
The investigators examined the relationship between the outcome with chest x-ray severity score, radiological features, and demographic and clinical parameters. The results supported using chest x-ray as a first-line triage tool in detecting COVID-19 pneumonia.
Toussie also has submitted, but not yet published, a manuscript on the value of a negative chest x-ray in predicting mild courses of COVID-19 that can be managed on an outpatient basis.
"X-ray is definitely useful for detecting COVID," Toussie added. "During the height of the epidemic in New York, the positive predictive value of opacities seen on x-ray was certainly high. After all, so many patients had COVID at the time, and patients without COVID were, for the most part, staying home. So the x-ray findings were highly specific."
But radiologists should be careful about using x-ray for diagnosis, as mild faint opacities could be missed. Her group's study showed, however, that patients without visible opacities seen on x-ray can be safely discharged from the emergency department and managed at home.
"However, now that there are so few cases of COVID in New York, the specificity of opacities on x-ray is much lower and are more likely to be caused by something other than COVID," she said. "In areas with high disease prevalence, the x-ray will be much more useful. Still, a laboratory confirmatory test is recommended for detection, not the x-ray."
Easy and quick
Additional backing for x-ray use during COVID-19 comes from a large public trauma hospital in Melbourne, Australia. Zoe Brady, PhD, chief physicist in the radiology and nuclear medicine department at Alfred Health, confirms that x-ray is easy, quick, and inexpensive to use.
"CXR [chest x-ray] is utilized as a baseline screen in patients presenting to the ED with symptoms suggestive of COVID-19 pneumonia. Mobile CXR doesn't involve moving the patient and potentially infecting or exposing the rest of the department," Brady said in an email to AuntMinnie.com.
Brady finds x-ray easier and quicker to use than CT.
"Repeat CXR is performed in a known COVID patient if there is respiratory decline to assess for complications, such as ARDS [acute respiratory distress syndrome], CCF [congestive cardiac failure], or pneumothorax," she added.
Still, Brady is aware of the limitations of chest x-ray, including its lower sensitivity compared with both RT-PCR and CT.
"CXR may be normal in the early stages postonset of symptoms or in asymptomatic patients," she said. "CXR findings peak quite late at 10 to 13 days after symptom onset, compared with CT at 6 to 13 days."
One challenge, though, is the lack of scientific evidence at present about the specificity of so-called "COVID-19 typical" lung findings, according to Brady. The typical findings on chest x-ray described for COVID-19 pneumonia in patients with high pretest probability of the disease include bilateral peripheral opacities (ground glass, consolidation, or a combination of both), with the lower zone being predominant, she indicated.
In addition, there is much overlap between the chest x-ray findings of COVID-19 pneumonia and other pulmonary processes -- both infectious (influenza and community-acquired pneumonias) and noninfectious (organizing pneumonia), she explained.
Complementary with CT
Meanwhile, x-ray and CT can complement each other in diagnosing COVID-19, according to a letter published June 15 in the American Journal of Roentgenology by Dr. Nicola Flor of Luigi Sacco University Hospital in Milan and colleagues.
"In our opinion, detailed descriptions of the CT findings of lung damage caused by COVID-19 may facilitate the interpretation of chest radiographs obtained in the same setting," Flor and colleagues wrote.
They further noted that only a few available studies are focused on the role of chest x-ray in the COVID-19 pandemic.
Flor indicated that chest x-ray findings, in combination with clinical findings and lung ultrasound, can help clinicians make a COVID-19 diagnosis in the ER while waiting for RT-PCR test results. She highlighted the advantages of x-ray versus chest CT -- lower costs, lower radiation dose, and lower risk of contamination for nurses and technicians, in particular in settings with a high prevalence of disease.
"But CXR is less sensitive than chest CT. Thus, CT could be useful in suspected patients with negative CXR, in particular in low prevalence settings," Flor said in an email.
Flor emphasized imaging's diagnostic role in addressing the pandemic, even with growing availability of RT-PCR testing.
"The diagnosis of pneumonia COVID-19 should result from a combination of clinical, laboratory, and imaging findings," Flor stated. "Even if there is a lack of data about RT-PCR accuracy, we know that its sensitivity isn't 100%, and thus there is the possibility of false-negative RT-PCR results. We have seen some cases of clear discrepancy between positive clinical and radiologic findings and negative consecutive RT-PCR."