Add breast biopsy procedures to the list of imaging tests that could be affected by new Medicare physician payment rates scheduled for 2014. Breast care advocates have weighed in against the proposed rates, charging that they could shift breast biopsies away from private-practice sites and into hospital settings.
In July, the U.S. Centers for Medicare and Medicaid Services (CMS) proposed new payment rates for its Medicare Physician Fee Schedule (MPFS) that included reductions for global reimbursement -- that is, payments for procedures performed in the freestanding office setting. The proposal has raised the ire of many radiology professionals who believe it cuts reimbursement for imaging studies on top of cuts that have already taken place over the past several years.
Now, the American Society of Breast Surgeons (ASBS) and the Society of Breast Imaging (SBI) have joined the chorus of opponents to the 2014 MPFS rates. The societies believe the cuts would result in insufficient reimbursement for percutaneous biopsy and could significantly affect the ability of physicians in private practices (also known as nonfacility settings) to offer these procedures.
"The 2014 values do not provide sufficient reimbursement to cover equipment, supply, staffing, and operational costs in the nonfacility setting -- the site of care that served over a third of Medicare beneficiaries who required vacuum-assisted biopsy in 2011," ASBS wrote in a letter to CMS.
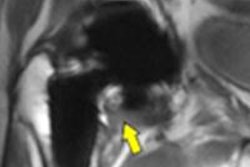
Image-guided percutaneous biopsy has become the procedure of choice for most breast lesions detected with imaging that require tissue diagnosis. As the majority of breast biopsies are benign, percutaneous biopsy eliminates the need for an unnecessary surgical procedure for diagnostic purposes, according to SBI, and its advantages include less scarring, fewer complications, faster recovery, less cost, and similar accuracy. Percutaneous biopsy can confirm the diagnosis of malignant disease and lead to a greater likelihood of obtaining clear margins at breast surgery.
"The proposed changes in the global reimbursement and MPFS will result in insufficient reimbursement for percutaneous biopsy procedures and will weigh significantly on physicians' ability to offer these procedures in the [private-practice] setting, creating an economic incentive for clinicians to take women to the operating room for a diagnosis via open-surgical biopsy," wrote Dr. Murray Rebner, president of SBI, in a letter sent to CMS.
In the proposed 2014 rule, CMS plans to issue new CPT codes that will bundle image-guided breast biopsy services with localization devices. (Code pairs identified as being performed together 75% of the time or more are considered for bundling.) The new codes will be created to describe breast biopsy procedures that include imaging guidance as well as placement of localization devices and imaging of the specimen when performed, according to an analysis conducted by the American College of Radiology (ACR).
CMS will also create new codes to report the placement of clips and other breast localization devices without biopsy or during aspiration procedures, ACR wrote. Although the proposed rule does not specify the new codes, it does assign new values for relative value units and associated reimbursement to the existing codes.
Historically, these procedures have had component-based coding in the freestanding setting. The proposed 2014 bundling and issuing of new codes makes it likely that there will be dramatic reductions in overall reimbursement for breast biopsy, according to both ASBS and SBI. For example, reimbursement for ultrasound-guided vacuum-assisted biopsy (VAB) procedures performed in the global setting (codes 19103, 76942, 19295, and 76645) would be reduced by 25% compared to 2013 amounts. Stereotactic VAB procedure reimbursement would be reduced by 14%. And the relative value units for the practice expense (PE) in the nonfacility setting would be reduced by 43% for ultrasound VAB and 35% for stereotactic VAB.
How would these reductions affect clinical practice? They'd make it challenging for private-practice physicians to pay their bills, according to Rebner.
"If reimbursement for image-guided core-needle biopsy and vacuum-assisted biopsy are dramatically reduced, it may make the provision of vacuum-assisted biopsy and the placement of a tissue marker for these procedures financially too burdensome for physicians practicing in a global setting," Rebner wrote.
ASBS urged CMS to study the impact of the proposed reductions in payments for these services, including shifts in site of service that could follow as patients may be forced to receive breast biopsy procedures in hospital outpatient departments, potentially resulting in increased travel times, time to diagnosis, and costs. In addition, reductions of this kind in reimbursement for percutaneous breast biopsy would create an economic disincentive for surgeons in the private-practice setting, who would no longer be able to afford these services because the costs associated with performing the procedures cannot be recovered, according to ASBS.
"Although we recognize that surgeons will always 'do the right thing' for their patients, the 'right thing' is for them to continue to stay in practice and take care of their patients," ASBS wrote. "No one can maintain a viable practice if expenses cannot be met."
CMS is taking comments on the rule until September 6.