Putting a quality improvement initiative in place to develop and reinforce critical test results communication can improve a department's performance by more than 60%. This not only helps patient care, it protects radiologists from malpractice suits, according to a study published this month in Radiology.
Researchers from Brigham and Women's Hospital evaluated the effects of a four-year initiative to implement and monitor a critical test results communication policy in the radiology department. They found that adherence to the policy -- and, therefore, more effective critical results reporting -- increased from 28.6% at the beginning of the period to 90.4% by the end of the study (Radiology, June 2011, Vol. 259:3, pp. 802-807).
Poor critical results reporting means more exposure to malpractice suits, according to contributing author Dr. Luciano Prevedello and colleagues.
"Delays and failure in communicating critical results pose threats to patient safety and are a leading source of medical malpractice claims in radiology," they wrote.
The group conducted a quality improvement initiative between February 2006 and January 2010, basing the program on recommendations from the Joint Commission, the American College of Radiology (ACR), and the Massachusetts Coalition for the Prevention of Medical Errors.
For the study, a critical result was defined as a finding that requires direct notification of a member of the patient's care team, including a new or unexpected radiologic finding that could result in illness or death if not addressed, or an interpretation that distinctly differs from a preliminary reading already communicated.
Three categories defined appropriate notification time parameters for critical results:
- Red alerts required notification of the patient's care team within an hour of the finding's discovery.
- Orange alerts required notification of the patient's care team within three hours of discovery, and included findings that could result in death or illness if not treated within two to three days.
- Yellow alerts required notification of the patient's care team within three days, and included findings that could result in death or illness if untreated, but they were not immediately life-threatening.
The quality initiative also outlined an escalation process in the event a radiologist was unable to reach a member of the patient's care team within the timeline for each alert level. The process included a description of the mode the communication should take (e.g., red and orange alerts required face-to-face or telephone contact), and a process for documenting in the radiology report the communication that had occurred.
Prevedello's team mounted posters describing the new guidelines in each radiology reading room. Results of periodic performance reviews were published on the department's Web-based dashboard and in the hospital's balance scorecard.
"Radiology leadership took an active role in communicating the initiative to all members of the radiology staff," the authors wrote. "No financial incentives were attached to performance during the quality improvement initiative period."
During 21 quality reviews, 16,983 (1%) of 1,489,951 total radiology reports were evaluated. Of these, 10%, or 1,628, were found to contain critical results according to the quality improvement initiative policy. Of those reports that failed to adhere to the critical results reporting policy, failure to appropriately document communication of critical findings was the most frequent cause (82%), while failure to communicate findings in the required time frame was less frequent overall (18%).
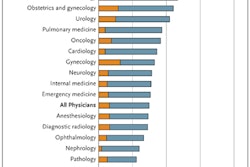
The percentage of reports considered to contain critical findings varied according to subspecialty, according to Prevedello and colleagues.
|
|||||||||||||||||||||||||||||||||||||||
| Data courtesy of RSNA. |
Putting a critical results reporting policy in place is necessary but not necessarily easy, according to the authors. It was labor-intensive to create alerts for the large number of imaging results that were considered critical (nearly 10%); to communicate with referring physicians using a paging system, which interrupted workflow; and to collate the performance review data.
"We achieved significant and sustainable improvements in physician adherence with a comprehensive policy on communication of critical imaging test results ... [but] achieving this success required substantial work effort," Prevedello and colleagues wrote. "Automated critical results management systems integrated into the radiologist's and the referring physician's workflows may further improve communication."