Failure to effectively communicate test results increases the risk of medical malpractice suits, according to a new study in the November issue of the Journal of the American College of Radiology. And even if radiologists are fifth on the list of primary responsible specialists in these suits, they are the first named as secondary responsible specialists.
Researchers at State University of New York (SUNY) Downstate Medical Center found that the growth in diagnostic test volume has led to a corresponding increase in reportable results -- thus exposing specialists such as radiologists to more medical malpractice risk (JACR, November 2011, Vol. 8:11, pp. 776-779).
"Between 1996 and 2003, total malpractice payments related to errors in diagnosis increased by approximately 40%," wrote lead author Dr. Brian Gale and colleagues. "In some cases, juries have broadened radiologists' responsibility to notify reportable findings to include patients."
The researchers sought to define the extent of malpractice costs related to communication failures in test result notification and to determine if these costs were increasing. The group found that claims payments increased at the national level by an average of $4.7 million annually, and communication failures played a role, accounting for 4% of cases by volume and 7% of the total cost.
Gale's group used National Practitioner Data Bank (NPDB) claims data from 1991 to 2009. NPDB operates under the U.S. Department of Health and Human Services; in 2010, it made a public-use file available that includes more than 850,000 entries for malpractice awards and disciplinary actions against physicians and other professionals between September 1990 and September 2010. The group also used Controlled Risk Insurance Company/Risk Management Foundation claims data for 2004 to 2008 for the study. This foundation is under the purview of the Harvard Medical Institution.
The study examined three reasons of action for medical malpractice suits:
- Communication problems between practitioners
- Failure to instruct or communicate with the patient or the patient's family
- Failure to report on the patient's condition
From the NPDB data, total indemnity payout across all medical specialties for U.S. claims related to these three reasons of action increased from $21.7 million in 1991 to $91 million in 2010. Gale's team performed linear regression analysis on the data and found that claims payments increased at the national level by an average of $4.7 million annually -- and the NPDB statistics underestimate the cost of malpractice litigation because they do not include costs of going to court or settling out of court.
NPDB communications awards accounted for an increasing proportion of total U.S. malpractice awards for all providers, increasing by a factor of 1.7, from 0.93% in 1991 to 2.31% in 2009.
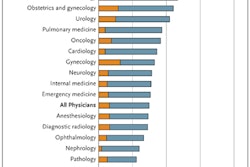
According to the Controlled Risk Insurance Company/Risk Management Foundation claims data, issues related to communication of test results were key contributors to 306 of the 8,417 claims recorded between 2004 and 2008; among these 306 malpractice cases, there were 396 instances of communication failure. Overall, malpractice cases in which communication failures played a role accounted for 4% of cases by volume and 7% of total cost. Radiologists were named as the primary responsible defendants in 7.8% of cases, although they were identified in 24% of cases as the secondarily involved practitioner.
|
Even if the reliability of reportable test results remained the same, the fact that the volume has increased exponentially would suggest an increase in notification failures, the authors wrote. But expectations regarding what is "reliable" have changed as well.
"The advent of increasingly efficient diagnostic modalities, the Internet, additional bandwidth, and numerous new channels to communicate a variety of data may have led to expectations of increasingly reliable communications of medical data between physicians and to patients," they wrote.
It's up to healthcare organizations to put clear policies in place that define the responsibility of reporting and referring providers to ensure patient follow-up, the team concluded. There are now commercially available systems designed to deliver test result notifications to referring clinicians and patients efficiently and to generate delivery receipts, in an effort to shorten notification intervals and avoid missed communication. And these systems can also help if a radiologist does encounter a malpractice suit.
"Delivering diagnostic test data to clinicians and patients more rapidly can facilitate earlier treatment, reduce morbidity, and shorten length of hospital stay," Gale and colleagues wrote. "If necessary, reports from automated notification systems can serve as documentary evidence of test result notification in litigation."