Aortic Rupture: (Pseudoaneurysm or Traumatic Aortic Laceration)
View cases of traumatic aortic laceration
Clinical:
An aortic laceration is an intimal tear that varies in depth, with transmural extension (aortic rupture or transection) being the most severe form [11]. The adventitia is intact in about 60% of cases which aids in the development of a pseudoaneurysm that delays complete rupture [11]. Traditionally, aortic laceration was felt to be secondary to sheering forces generated by abrupt thoracic deceleration at the points where the fixed aortic root and descending aorta join the mobile arch. More recently, it has been suggested that traumatic rupture may be caused by pinching of the aorta between the anterior and posterior components of the bony thorax when the chest is compressed [1]. Between 30% to 50% of patients with acute traumatic aortic injury will show no external sign of direct chest injury (ie: chest wall contusion or abrasion, or palpable rib/sternal fracture) [11].
Slightly fewer than 1% of all blunt trauma patients have a traumatic aortic laceration. However, for affected patients the prognosis is grave and between 80-90% of patients with traumatic aortic rupture die before emergency treatment can be instituted [11]. Of those that survive the injury, 50% will die within 24 hours without repair [11]. For those who survive transport to a hospital, 80% live to be discharged if given appropriate treatment.
Tears tend to occur at sites of fixation such as: 1- The ligamentum arteriosum (aortic isthmus), just distal to left subclavian, which is the most common site (95%); 2- the ascending aorta just beyond the aortic valve (5%) which is covered by pericardium and usually results in hemopericardium and death (incidence of ascending aortic injury is higher in autopsy series [20-25%]); and 3- the diaphragmatic hiatus (1% to 3%). Multiple aortic lacerations can be seen in 6% to 20% of cases [11]. Concomitant aortic branch vessel injury occurs in 4% to 10% of cases [11].
Treatment of aortic post-traumatic laceration is generally primary surgical repair. The mortality rate associated with emergent surgical treatment is 15-29%, in part due to the frequency of coexisting serious non-aortic injuries [6]. Post-operative paraplegia occurs in up to 25% of patients and is related to the duration of aortic cross-clamping [11]. Recently, endovascular stent-grafts have also been used for the treatment of acute and chronic traumatic aortic aneurysms. Stent-grafts may be particularly useful in patients with contraindications to conventional surgery. Because the stent requires a 18-24 F delivery system, surgical exposure of the aorta or iliac vessels is sometimes required to obtain vascular access. Complications include obstruction of the take off of the left subclavian artery and perigraft leak. [6]
About 2% to 5% of patient with untreated traumatic aortic injury survive and develop a chronic pseudoaneurysm- most commonly in the region of the ligamentum arteriosum [9,11]. Rupture can occur in up to 25% of chronic pseudoaneurysms [6]. Rupture can be fatal- 10 year survival for those who decline surgical repair is 66%, but is 85% for those who undergo treatment. [2]
X-ray:
Plain films: The greatest value of the frontal chest radiograph is not in suggesting aortic injury, but in excluding it. A truly normal frontal CXR has a 98% negative predictive value for aortic injury [9,10] (96% for a supine view). Unfortunately, the specificity of an abnormal exam is poor [11]. In fact, the incidence of aortic rupture in patients evaluated by angiography solely because of an abnormality found on the frontal CXR, is only between 10-20%.
Plain film findings which suggest aortic disruption include (an upright frontal film is essential, but unfortunately difficult to obtain in trauma patients): 1- Transverse width of the mediastinum greater than 8 cm just above the aortic knob; 2- Mediastinum to chest width ratio greater than 2.5 ; 3- Aortic contour abnormality with blurring of the outline of the descending aorta; 4- Aortopulmonary window opacification; 5- Widened left paraspinal stripe; 6- Depression of the left mainstem bronchus more than 40 degrees below the horizontal; 7- Tracheal deviation to the right of the T4 spinous process; 8- NG tube deviation to the right at the T4 spinous process; 9- Right or left pleural cap; 10- Left hemothorax without rib fracture; 11- Right paratracheal stripe thicker than 5mm; 12- First rib fracture is also a marker of severe chest trauma and up to 18% of patients with aortic tears are also noted to have a fracture of the first rib. Therefore, the following recommendations are reasonable- patients with a grossly abnormal chest radiograph AND an appropriate mechanism of injury for rupture should have an arteriogram performed if they are hemodynamically stable. Patients who are hemodynamically stable and have equivocal radiographic findings or a mechanism of injury that seems unlikely to have resulted in aortic injury, should proceed to CT of the thorax or Transesophageal Sonography. [2]
Computed Tomography:
CT is less invasive, readily available in most hospitals at all hours, and can result in
substantial cost savings when evaluating patients for suspected aortic injury [16]. CT
scans should not be performed in hemodynamically unstable patients, in patients
with obvious plain film radiographic evidence of aortic injury (unless the surgical team
will accept the CT findings and not require further angiographic evaluation), or in
patients in whom the mechanism of injury strongly suggests aortic injury (controversial-
some authors would screen with CT). These patients should instead proceed directly to
aortography. In the absence of these criteria, CT can be used as a screening tool,
especially in those patients undergoing CT examination for other injuries [4,5].
A normal CT scan essentially excludes aortic injury (ie: sensitivity and negative predictive value approach 100%)- fewer than 1% of patients with a normal CT are found to have an aortic rupture on subsequent aortography [3,16]. Unfortunately, CT has a lower specificity because the scan findings are completely normal in only about 25% of patients. The false positive rate for CT in the detection of aortic injury has been reported between 0-39% [10,16].
The accuracy of CT for the detection of branch vessel injury has not been extensively studied.
Exam: Helical CT is superior to conventional CT imaging for the detection of aortic injury [14]. The scan should begin at the level of the diaphragm and progress cephalad to above the aortic arch. Other authors recommend beginning imaging at the base of the neck and extending inferiorly to the diaphragm [11]. Contrast is administered at a rate of 2 to 3 mL/sec for a total of 100 to 150 cc. A right arm injection is prefered to decrease streak artifacts that occur as the contrast bolus traverses the thoracic inlet vessels [16]. A scan delay of 20 to 30 seconds or a smart prep can be used to determine the best time for imaging. Images are acquired helically with 5 to 7 mm thickness, a pitch of 1.0-2.0, and are reconstructed at 2.5 to 3.5 mm intervals (some authors recommend a 50% overlap [11]). Some authors advocate the use of thinner images (3 mm) and thinner reconstructions (1.5 mm) through the aortic arch with 7-8 mm thick slices through the remainder of the aorta [16]. Parasagittal reformatted left anterior oblique images can be created to evaluate the arch for contour abnormalities [10].
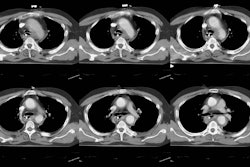
Findings: Direct findings on CT of aortic transection include irregular contour or a change in caliber of the aortic lumen at the level of the isthmus- often a focal outpouching consistent with a pseudoaneurysm can be seen in association with this finding. An intralumenal flap appears when the wall of the aorta is outlined by contrast material because of a contained rupture. Up to 17% of aortic tears can occur without significant mediastinal hematoma [9].
The presence of a mediastinal hemorrhage is considered indirect evidence of an aortic transection. The hematoma is usually periaortic and may extend inferiorly along the descending aorta. The hemorrhage may appear as streaky increased density within the mediastinal fat or be a more focal collection of blood. Most authors would agree that if a mediastinal hematoma is present, the patient should undergo aortography regardless of the appearance of the aorta on CT [9]. Unfortunately, the presence of a mediastinal hematoma does not confirm the diagnosis of aortic transection as it may also be seen in blunt trauma patients for other reasons such as sternal or thoracic spine fracture, or venous bleeding (ie: the finding is very sensitive, but not specific for aortic injury). In fact, up to 97% of angiograms performed on patients with only mediastonal hematoma, but no aortic abnormality, are negative [10]. Some authors now recommend that patients with isolated, small mediastinal hematomas separate from the aorta and a normal appearing aorta at helical CT do not require angiographic evaluation [12-15]. Instead, these patients can be followed clinically and with plain film radiographs for a 4 to 6 month period [12].
Difficulties in exam interpretation may occur secondary to normal thymus (mimics hematoma), the pulmonary artery, periaortic atelectasis (mimics periaortic hematoma), motion, or partial volume effects [11].
Angiography: Angiographic findings of thoracic aortic injury include the identification of a pseudoaneurysm, intimal or media tear, or rupture with contrast extravasation. Subtle lesions may be missed if two views (lao and ap) are not obtained. False positive exams occur in approximately 1% of cases [11]. A congenital ductus diverticulum may cause a false positive exam. Findings which help to identify a ductus diverticulum are its smooth contour, obtuse angles with the aortic wall, and the absence of overlapping density at its edges.
Transesophageal echocardiography (TEE): TEE can be used in the evaluation of aortic injury. Direct signs of aortic injury include depiction of an aortic flap or pseudoaneurysm, or an aortic wall hematoma [11]. Atherosclerotic disease can produce false-positive exams. Findings which suggest the presence of a mediastinal hematoma include a distance of more than 3 mm between the probe and the aortic wall; a double contour of the aortic wall; or an "ultrasound signal" between the aortic wall and visceral pleura [11]. Overall data from recent studies suggest a sensitivity of 57-63% and a specificity of 84-91%. The exam is technically inadequate in about 15% of patients, is invasive, requires technical skill, and has a 2.9% complication rate [11].
REFERENCES:
(1) Semin Ultrasound CT MR 1996 Apr;17(2):119-141
(2) Radiographics 1997; 17: 27-45
(3) J Thorac Imag 1996; 11: 39-45
(4) AJR 1994; 162(5): 1047-1052
(6) Radiology 1997; 205: 657-662
(8) AJR 1998; Wong YC, et al. Periaortic hematoma on helical CT of the chest: A criterion for predicting blunt traumatic aortic rupture. 170: 1523-1525
(9) Radiographics 1998; van Hise ML, et al. CT in blunt chest trauma: Indications and limitations. 18: 1071-1084
(10) Radiographics 1998; Kuhlman JE, et al. Radiographic and CT findings of blunt chest trauma: Aortic injuries and looking beyond them. 18: 1085-1106
(11) Radiology 1998; Patel NH, et al. Imaging of acute thoracic aortic injury due to blunt trauma: A review. 209: 335-348
(12) Society of Thoracic Radiology Course Syllabus 1999; Fishman JE. Imaging of aortic and great vessel trauma. p. 75-84
(13) Society of Thoracic Radiology Course Syllabus 1999; Primack SL. CT in blunt chest trauma: Indications and limitations. p. 87-98
(14) AJR 1999; Fishman JE, et al. Direct versus indirect signs of traumatic aortic injury revealed by helical CT: Performance characteristics and interobserver agreement. 172: 1027-1031
(15) Radiology 1999; Dyer DS, et al. Can chest CT be used to exclude aortic injury? 213: 195-202
(16) AJR 2001; Parker MS, et al. Making the transition: The role of helical CT in the evaluation of potentially acute thoracic aortic injuries. 176: 1267-1272