Early tests on brain cancer patients show significant promise for the use of MR fingerprinting to produce previously unattainable quantitative information in a short time, according to Dr. Siegfried Trattnig of the Medical University of Vienna, where new research on 10 volunteers has been carried out since ECR 2015.
 Dr. Siegfried Trattnig sees a "paradigm shift" from qualitative to quantitative imaging. Image courtesy of Medical University of Vienna/E. Hammerschmid.
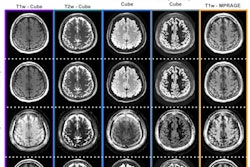
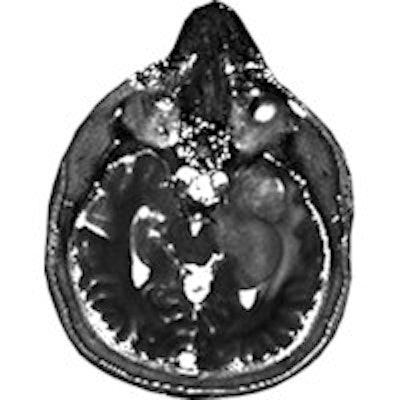
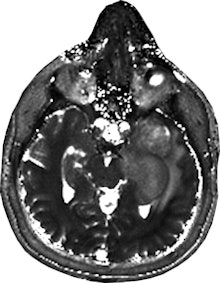
Dr. Siegfried Trattnig sees a "paradigm shift" from qualitative to quantitative imaging. Image courtesy of Medical University of Vienna/E. Hammerschmid.The results using an advanced MR imaging protocol and MR fingerprinting showed that the T1 and T2 mapping of tissue provided by fingerprinting was "better visualized" than in the standard protocol, said Trattnig, medical director of the university's Centre of Excellence in High Field MR and the chairman of the European Imaging Biomarkers Alliance (EIBALL). The testing was conducted using five patients with malignant brain tumors and an equal number with low-grade gliomas.
"It's my impression that we see more changes by using MR fingerprinting based on T1 and T2 maps on this quantitative data. And looking into the tumor, you see more details that are not shown on standard imaging," he explained, emphasizing that the results of the Austrian university's 2015 tests are only preliminary.
ECR delegates have the opportunity to learn more about MR fingerprinting during today's discussion of imaging biomarkers and their promise in the treatment of cancer and other chronic diseases.
Fingerprinting has yet to be tested in clinical settings, and Trattnig acknowledges that there are divergent views amongst radiologists on whether the technique can successfully deliver stable and robust quantitative data. Initially he was skeptical about the clinical potential of MR fingerprinting, but he now sees it as potentially transformational. Instead of a standard MR protocol that provides qualitative information, fingerprinting can automatically provide a fast sequence that delivers quantitative diagnostic data as well.
"I believe that MR fingerprinting will help the radiological community to make this paradigm shift from qualitative to quantitative imaging, and also to use quantitative data more in their daily routine work," said Trattnig, adding that the information provided from fingerprints could be used to tailor treatment to patient needs.
The technique is also fast: Results from the Vienna tumor study showed that the standard advanced MR imaging protocol took one hour for each patient, while the fingerprinting protocol could be done in five minutes.
MR fingerprinting could be advantageous in other ways. Preliminary results suggest that there was low variability of the T1 and T2 relaxation times over multiple examinations of volunteers in Vienna, with the potential to accurately monitor and evaluate the progress of treatment, or even provide clues in the early detection of cancer. In addition, fingerprinting may also yield cost savings because of the reduced mapping time involved, and it is based on software that can be added to existing MR equipment, said Trattnig.
The Vienna researchers have been collaborating with other colleagues, including Mark Griswold, PhD, of the department of radiology at Case Western Reserve University in Cleveland, Ohio, U.S., whose interest in MR fingerprinting helped spark the project with the European researchers. Griswold was a contributing author of an article published in the journal Nature in 2013 that identified MR fingerprinting as a way to obtain simultaneous quantification of tissue properties without a surgical procedure (Nature, March 2013, Vol. 495:7440, pp. 187-192). The authors also argued that fingerprinting has been shown to reduce measurement mistakes when teamed with pattern-recognition algorithms.
Apart from fingerprinting, ECR delegates will also learn about advances in the use of optical probes, nuclear probes and combinations of the two for tumour imaging, as well as gauging the effectiveness of cancer therapy. For instance, imaging using receptor-targeting peptides has been shown to predict treatment effectiveness.
Prof. Marion de Jong of the Erasmus University Medical Centre in Rotterdam sees targeted imaging as increasingly important in the field of theranostics, which combines diagnostic and treatment approaches to tailor patient care -- or what she describes as "the right treatment for the right patient at the right time and the right dose."
"In nuclear medicine the concept of theranostics is easy to apply and to understand, because of an easy switch of a diagnostic radionuclide to a therapeutic radionuclide on the same probe," said de Jong, who is based in the Erasmus MC's nuclear medicine department. This "switch" has the potential to both diagnose and stage tumors, as well as select the optimal therapy and dosage.
Originally published in ECR Today on 3 March 2016.
Copyright © 2016 European Society of Radiology