How does immediate AI-enabled patient triage on chest CT impact the lung cancer pathway?
It's a question researchers at University College London Hospitals NHS Foundation Trust and Canterbury Christ Church University have asked as part of their prospective, randomized, multisite trial currently open and underway in the U.K. Nearly 72,000 chest x-rays had been randomized as of November 25 (the study is open through December 31), with the two primary outcomes of the trial being time to diagnosis of lung cancer and time from chest x-ray to CT by prioritizing abnormals.
The largest share of chest x-rays comes from University Hospitals of Leicester (UHL) with 33,105 from 31,210 patients referred from primary care between October 2, 2023, and June 28, 2024, according to interim recruitment data shared by study lead Nick Woznitza, PhD, consultant radiographer and clinical academic at University College London Hospitals (UCLH). UCLH has produced 9,217 chest x-rays from 8,072 patients.
Scans undergo data cleaning, Woznitza explained to retain only scans necessary for compliance. So far, the analysis cohort consists of 68,647 consecutive chest x-rays for a current total of 64,505 patients, for the purpose of measuring impact with AI prioritization (35,251) using the software qXR from Qure.ai, designed to spot potential abnormalities on chest x-rays, and also without AI prioritization (33,396).
Within the interim results, Woznitza reflected the results as they relate to four categories: time to lung cancer diagnosis, time to CT, time to urgent referral, and time to treatment start in relation to 191 lung cancer cases diagnosed. And of the 191 cases, 89 were not prioritized by AI. The other 102 were prioritized.
While the median number of days from chest x-ray to the final diagnosis for the 89 cases was slightly lower (30) than the larger group (33.5), the team found no statistical difference, Woznitza reported during the talk.
However, time to CT as measured from 2,750 studies was a significant 27% shorter using AI prioritization, at 27 days versus 32 days, Woznitza said. Using AI prioritization also resulted in a slight reduction in the time to urgent referral at 10 days versus 14.
"When we looked at the CTs which were done based on the radiology report saying this is suspicious of cancer, please fast-track it, there was actually quite a difference," Woznitza said. "The difference actually held for those CT scans done after a noncancerous chest x-ray."
The study was approved by the East of England Research Ethics Committee, and more results are forthcoming.
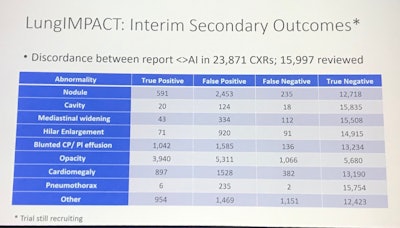
"We're going to have really rich information on the proportion of false negatives and positives," Woznitza as he closed his talk after a brief look at other measures, which are shown below.
This research is important because, despite the introduction of lung cancer screening, a majority of patients present through the symptomatic route when a chest x-ray is the most common first investigation, the investigators noted. Rapid diagnosis could be facilitated by correct identification of patients who would benefit most from an urgent CXR report and progression to urgent CT where indicated.
Ultimately, the LungIMPACT study will determine if AI helps identify chest x-rays from patients who will benefit most from same-day CT, triaging for an immediate review and report.
Others on the team include lead investigator David Baldwin, MD, chair of NHS England’s Clinical Expert Group for Lung Cancer and a respiratory consultant at Nottingham University Hospitals, cardiothoracic radiologist Indrajeet Das, MD, and Prof. Neal Navani and Arjun Nair, MD, radiologists at UCLH.
For full 2024 RSNA coverage, visit our RADCast.