Breast imagers will have a wide variety of scientific content in women's imaging to see at the RSNA 2020 virtual meeting. From efforts to personalize breast screening to cutting-edge techniques changing the way breast cancer is treated, researchers are working to improve the entire continuum of breast care.
Some of the most popular topics at the meeting will be the use of breast MRI and artificial intelligence (AI) for mammography, according to RSNA breast imaging subcommittee chair Dr. Fiona Gilbert from the University of Cambridge in the U.K. Attendees will also be able to learn about exciting new developments in ultrasound and the intersection of women's imaging and interventional radiology.
Below are three topics at this year's conference that experts believe researchers will be talking about at RSNA for years to come.
1. AI for women's imaging
AI is arguably the most popular topic at this year's RSNA meeting, according to Gilbert. She is particularly excited about its use to improve mammography and digital breast tomosynthesis (DBT).
"Individual practices can use an AI tool to have much more information about a batch of mammograms before they even sit down and start reading them," Gilbert said. "That's going to be hugely valuable."
 Dr. Fiona Gilbert.
Dr. Fiona Gilbert.For instance, AI can help radiology practices triage cases, Gilbert said. Practices can prioritize mammograms with the greatest likelihood of having cancer to be read in the morning, by multiple radiologists, or by imagers with the most experience. Cases with the least likelihood of having cancer can be read later in the day, by a single radiologist, or by newer radiologists.
Dr. Hannah Chung, an assistant professor of breast imaging at the University of Texas MD Anderson Cancer Center in Houston, also pointed to AI as one of the most exciting developments happening right now in women's imaging. Chung is particularly interested in research using AI to highlight lesions on ultrasound and MRI, since it can be relatively easy to flag inconsequential findings on these two modalities.
"Use of artificial intelligence to minimize these false positives holds promise to help us make better interpretive decisions," she said.
Another AI application Chung would like to see is the use of decision-tree algorithms that predict treatment response with the aid of imaging findings. It's very possible that will be a topic discussed at RSNA and other conferences this year or in the near future, as Gilbert thinks AI will continue to dominate the radiology landscape.
"We're going to see more of that in terms of feasibility, implementation, and impact on patient care," Gilbert said.
2. Better breast screening
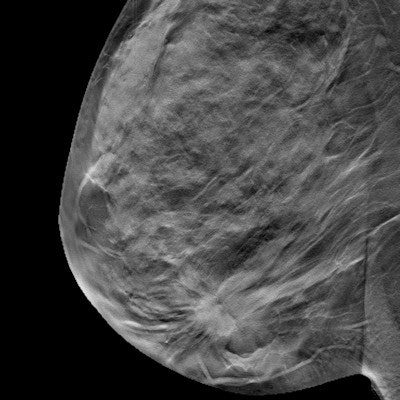
Breast screening is always one of the most talked-about topics in breast imaging. Lately, that discussion has largely revolved around DBT -- and for good reason, noted Gilbert.
"It's one of those rare situations where a new technology not only increases the specificity of a test, but the sensitivity as well," she said.
Both Gilbert and Chung have no doubts about the benefits of DBT, particularly its ability to reduce patient recalls. But the technology also has its drawbacks. Notably, mammography, DBT included, has limited ability to detect cancers in women with high breast density.
As a result, researchers and clinicians are looking for more sensitive alternatives. Most often, their top choice is MRI.
 Dr. Hannah Chung.
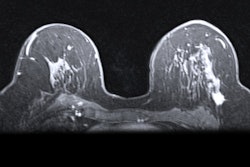
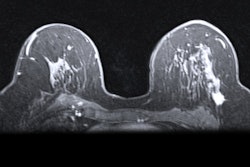
Dr. Hannah Chung."The reason that there's so much interest in breast MRI is that it's the most sensitive imaging modality we have," Gilbert said. "It's the best technique for picking up breast cancer."
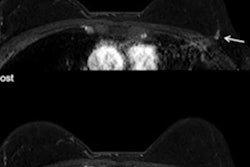
MRI's unparalleled sensitivity could be why the modality is still a "hugely popular" topic at this year's conference, according to Gilbert. She highlighted a number of applications drawing interest among the research community, including abbreviated protocols to shorten scan time and the use of MR for dense breasts.
However, MRI has its own drawbacks. Chung noted that breast MRI has a long scan time, and some patients may have issues with the closed physical space of the magnet bore. In addition, the long-term effect of repeated gadolinium contrast is unknown, a problem that could be compounded with the use of MRI for screening.
For Gilbert, the biggest drawback of MRI is its cost. This is perhaps most notable in the Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial, a recent randomized controlled trial out of the Netherlands. Despite overwhelmingly positive results in favor of MRI as a screening modality, the Dutch authorities are hesitant to move forward with it, Gilbert said.
Despite its downsides, MRI will still have uses in screening in the future. Even today, patients with a high breast cancer risk, including BRCA gene carriers, are offered breast MRI screening exams. Any advancements to reduce that cost would open breast MRI screening to more people, Gilbert noted.
"An abbreviated examination is about a third of the time of a full-protocol examination, and it's much faster to read," she said. "If you think about it very roughly, it's about a third of the cost of a full-protocol examination. So that means you could offer it more widely."
However, it's clear that MRI can't be the primary screening modality for most women. One alternative could be whole-breast ultrasound, another topic that will be discussed at this year's conference.
Gilbert sees ultrasound becoming a more prominent tool in the future for both screening and supplemental imaging, and she believes researchers will continue to unveil developments. But both Chung and Gilbert pointed to contrast-enhanced digital mammography (CEDM) as the more likely MRI alternative for women with dense breasts.
"Of all tests, CEDM has shown great promise, as it combines anatomy and physiology, is generally well tolerated by most patients, and is overall a low-cost examination," Chung said.
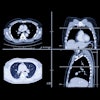
Like a contrast CT exam, CEDM utilizes digital mammography with an iodinated contrast agent. The main advantage of CEDM is that it has the same indications as MRI but is drastically cheaper.
"It's a terrific technique, and it looks as though it's almost as good as MRI," Gilbert said. "It's very promising."
Gilbert's department is currently conducting a multicenter, randomized clinical trial to compare CEDM, abbreviated MRI, and whole-breast ultrasound screening in women with dense breasts. So far, the team has recruited the first 600 patients in hopes of figuring out which modality will be the most cost-effective and feasible for long-term use.
The study is a step toward a future where a woman's primary screening modality will be personalized based on her individual risk factors. For instance, breast radiologists may recommend MRI for women with the highest cancer risk, CEDM for those with moderate risk, and DBT for the general population, Gilbert noted.
"People are going to be thinking more about taking a risk-adaptation approach in terms of looking at an individual's personal risk of developing breast cancer -- and looking at what might be more appropriate imaging modalities for that individual," she said.
3. Interventional opens door to new breast therapies
Another topic at this year's conference will be the use of interventional radiology techniques to improve treatment for breast, gynecological, and other cancers, according to Dr. Ronald Arellano, an interventional radiologist and chair of the RSNA subcommittee for vascular and interventional radiology.
 Dr. Ronald Arellano.
Dr. Ronald Arellano.As the field has advanced, interventionalists are now able to couple interventional radiology (IR) techniques with immunological and molecular data in order to treat tumors at a more detailed and refined level. This expanded IR toolkit includes numerous advanced therapies, including cryoablation and radioembolization.
While Arellano predicts that physicians across the board will increasingly embrace newer IR techniques, he also said that healthcare professionals who focus on women's cancers, notably gynecologic oncologists and breast oncologists, have been especially open to an expanded use of IR therapies.
Arellano is very encouraged by the willingness of these physicians to pursue new treatment options for patients with oligometastatic disease, and he gave a few examples of how this trend is playing out. For instance, a woman with breast cancer who develops a tumor in her liver may undergo localized regional therapies, whereas in the past, she would have almost exclusively received chemotherapy.
"Even though it is defined as metastatic and their overall survival may not be that good, we have this technology now. What's the harm in giving it a try?" Arellano said. "We can do our best to locally control disease, then pull the trigger on chemotherapy if we need it later."
The breast experts agreed with the promise of interventional techniques to better treat breast cancer and its metastases. However, both Chung and Gilbert were more excited about the use of emerging interventional techniques to manage small, low-grade breast cancers and ultimately avoid invasive surgeries.
"We're already seeing different techniques with ablation, cryoablation, etc., coming through for breast lesions," Gilbert said. "We're going to see more of that."
Physiology-based imaging
The use of imaging to better understand the tumor environment is a topic that may not be as popular at this year's RSNA meeting, but it will surely be a discussion point at future ones. Chung defined this type of imaging as physiology-based imaging.
The crux of physiology-based imaging is to answer the following question: Can imaging differentiate the various types of breast cancer based on specific features? By definition, it requires a multimodality approach, including the use of MRI, CEDM, molecular imaging, PET, and various radiotracers.
"We are already blending physiology and anatomy to a certain degree, which is a paradigm shift from strict anatomical imaging," Chung said. "However, payment models that incentivize and appropriately compensate for these exams are necessary before they are widely used."
Although they have a way to go, advanced physiology-based imaging tools appear promising to help physicians better understand the tumor environment and, ultimately, use this information to propose the most effective treatments and regimens for each patient. It's part of the larger trend of further personalizing medicine, including breast cancer treatment, noted Gilbert.
"It's one of the pieces of information that we kind of ignore when we're deciding what kind of chemotherapy patients should be getting," Gilbert said. "It's part of the information that's important for determining whether a cancer is going to grow and spread, or whether a cancer is going to respond to a particular type of treatment."
Programming schedule
Several breast imaging sessions can be found on the virtual RSNA 2020 program.
Sunday, November 29
- 10:00 a.m.-11:00 a.m. -- Science Session: Breast Imaging (MRI)
- 5:00 p.m.- 6:00 p.m. -- Education Session: Case-based Review of the Breast
Monday, November 30
- 8:30 a.m.-9:30 a.m. -- Science Session: Breast Imaging (Artificial Intelligence)
- 2:00 p.m.-3:00 p.m. -- Controversy Session: To Look or Not to Look -- Does Every Woman with Newly Diagnosed Breast Cancer Need Axillary Imaging?
- 3:30 p.m.-4:30 p.m. -- Education Session: Case-based Review of the Breast
Tuesday, December 1
- 2:00 p.m.-2:30 p.m. -- Image Interpretation Session: Chest and Breast
Wednesday, December 2
- 8:30 a.m.-9:30 a.m. -- Education Session: Essentials of Breast Imaging
- 3:30 p.m.-4:30 p.m. -- Science Session: Breast Imaging (MRI)
Thursday, December 3
- 2:00 p.m.-3:00 p.m. -- Education Session: AI in Breast Imaging
Friday, December 4
- 10:00 a.m.-11:00 a.m. -- Hot Topic Session: Integrated Diagnostics -- Risk Predictions of Breast Cancer
- 2:00 p.m.-3:00 p.m. -- Science Session with Keynote: Breast Imaging (Artificial Intelligence)
All events are listed in Central time.