When there's an unsuspected radiographic finding (URF) on a chest image, who makes sure that follow-up occurs? After dropping the ball for one patient, a center in Oregon has devised a relatively simple and inexpensive system to see that it doesn't happen again.
The systematized approach by the Veterans Affairs Medical Center in Portland has also confirmed the general value of following up on URFs -- findings unrelated to the reason for the requesting clinician's order.
One of every 17 URFs followed by the Portland VA has turned out to be stage IA primary lung cancer -- an otherwise fatal tumor caught at a potentially treatable stage. The center's five-year experience with its clinical pathway is reported this month in the journal of the American College of Chest Physicians (Chest, May 2004; Vol. 125:5, pp. 1753-1760).
The Portland facility set up its pathway in 1996, after diagnosing a patient with nonresectable lung cancer. Years earlier, the same patient had a routine preoperative chest x-ray in which the radiologist noted a vague abnormality where the lung cancer was later diagnosed.
"That prompted us to think that we should have better mechanisms, so that any abnormality that a radiologist is concerned about has an opportunity for follow-up," said Dr. Mark Deffebach, an associate professor of medicine at Oregon Health Sciences University, staff physician at the Portland VA, and co-author of the new study.
Even when the radiologist directly communicates an unsuspected finding to the referring physician -- as recommended by the American College of Radiology for urgent findings -- the referring physician is often a procedure specialist or urgent-care physician who isn't the best source to manage a follow-up, Deffebach noted.
So the Portland VA opted for a simple system in which radiologists notify a nurse specialist of any URFs. The nurse collates all relevant clinical information for review by the pulmonary service consultation team. A preliminary follow-up plan is devised, and the patient's primary-care physician -- if they have one -- is alerted.
Any radiographic imaging study that shows a URF on the chest -- including shoulder x-rays or abdominal CT scans -- can be submitted for follow-up. Routine x-rays taken for cough, shortness of breath, worker's compensation checkups, etc. also provide a steady source of URFs, Deffebach said.
Routine chest radiographs at the Portland VA are taken with a CR system (Fujifilm Medical Systems USA, Stamford, CT); CT scans are performed using a four-detector LightSpeed scanner or a one-detector scanner (GE Healthcare, Waukesha, WI).
Between April 1, 1996 and March 31, 2001, the center followed up on 1,629 URFs noted by radiologists. The vast majority of URFs came from chest radiographs (1,359, or 83.4%) as opposed to CT scans (270 URFs, or 16.6%), although CT studies increased by 192% over the study period.
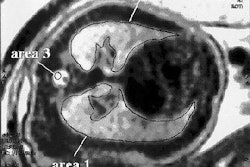
Most of the URFs (78%) were nodules or similar densities and opacities that were too small to be further characterized by the radiologist. The next most common URF category was abnormal shadows in the mediastinum or hila (10%). Upon follow-up, many of the findings were either resolved or not subsequently seen (39.5%), or proved stable over time (17.9%).
Another 32.8%, or 534, of the primary URFs (those seen on the initial image versus those discovered on follow-up imaging) were deemed clinically significant, and two-thirds of those required immediate treatment.
Half of the significant URFs turned out to be neoplasia, and many were caught at an early stage.
"One-third of the non-small cell lung cancers found by the URF pathway (33.7%) were at stage IA, the most favorable stage for responsiveness to treatment," the authors noted. In contrast, only 16.5% of the lung cancers diagnosed hospital-wide by the Portland VA over the same period were stage IA.
The annual cost of the pathway was calculated at $28,600, covering an extra 2.5 hours per week of pulmonary physician time and 10 hours per week for the nurse specialist. The calculation does not include the cost of additional imaging or other follow-up, which the authors argued would have been incurred sooner or later even without the pathway.
In addition, the pathway may save some imaging costs, as the nurse specialist is tasked with tracking down old films that can confirm the stability and insignificance of many URFs, Deffebach said.
"The major advantages of our pathway are that URFs do not go unrecognized and the efficiency of evaluation is, hopefully, improved," the authors concluded. "Our analysis of the costs suggests that they are a reasonable trade-off for the benefits gained."
By Tracie L. ThompsonAuntMinnie.com staff writer
May 28, 2004
Related Reading
Chest CT protocols reduce dose significantly, May 6, 2004
Chest x-ray benefits from CAD for spotting lung nodules, March 18, 2004
Lung nodule analysis makes progress, not perfection, March 5, 2004
Copyright © 2004 AuntMinnie.com