CT's value as a lung cancer screening tool may be outweighed by the potential risk of evaluating nodules that turn out to be benign, according to researchers from Johns Hopkins University in Baltimore.
Writing in the January 15 Journal of the American Medical Association, the group found that CT lung cancer screening saved a few lives compared to no screening, but at an unacceptably high cost per life saved (JAMA, January 15, 2003, Vol. 289, pp. 313-322).
"Past attempts to screen for lung cancer with intensive screening regimens and sputum cytology found no reduction in lung cancer-specific mortality, raising skepticism on whether lung cancer is amenable to early detection," wrote lead author Dr. Parthiv Mahadevia and colleagues.
Moreover, direct-to-consumer marketing and media coverage of government-funded CT trials have increased consumer demand for screening without proof that the tests save lives, they added.
There are an estimated 50 million current and former smokers in the U.S. between the ages of 45 and 75. Offering periodic annual screening to even half of this group would cost approximately $115 billion, according to the authors.
The group performed a decision and cost-effectiveness analysis from the societal perspective, simulating the clinical paths and health states of those who undergo screening compared to those who do not.
The investigators considered parameters such as age, smoking status, and the sensitivity and specificity of CT lung screening. They examined characteristics of the disease such as treatment, prognosis, and quality of life, and characteristics of the screening program itself, including efficacy and biases in screening. The research was based on published data, and on the National Cancer Institute's SEER (Surveillance, Epidemiology, and End Results) database.
The benefits of screening were calculated by comparing the absolute and relative difference in lung cancer-specific deaths. The group measured harms by calculating the number of false-positive invasive tests or surgeries per 100,000 individuals, as well as the incremental cost-effectiveness in quality-adjusted life years (QALY) saved.
Using this data, the group compared screening to no screening in 100,000 hypothetical current smokers. They then performed the same comparison in smokers who were in the process of quitting at the time of the screening, and in former smokers who had quit smoking five or more years before the screening exam.
Due to lead time bias inherent in screening and follow-up, the investigators assumed that 50% of non-small-cell lung cancers would undergo a downward stage shift. No shift was assumed for small-cell lung cancers due to their early metastatic nature and low probability of cure.
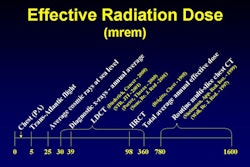
The model also assumed that radiation from screening exams would not lead to an increase in cancers, and that prognosis, as well as risks and costs of treatment, were similar for both screened and nonscreened individuals.
The calculations were based on known progression and screening-detection rates over 20 years: in all, 462,352 screening exams in current smokers. They estimated 3,615 lung cancer deaths among those who were screened, compared with 4,168 lung cancer deaths among those who had no screening.
The model showed that there were 553 (13%) fewer deaths among those who were screened, but those extra life years came at a high cost, both economically and in terms of risk. There were 1,186 invasive tests or surgeries for benign lesions in the screened group.
"The incremental costs consumed by screening ... (were) between $4,300 and $4,600 for all cohorts," the authors wrote. "However the incremental effectiveness of screening decreased with lower-risk cohorts."
- With screening, current smokers gained 0.039 QALY at $116,300 per QALY saved.
- Quitting smokers gained less: 0.008 QALY at $558,600 per QALY saved.
- Smokers who had quit more than 5 years before screening gained the least: 0.002 QALY at $2,322,700 per QALY saved.
In the U.S., $50,000 or less per QALY saved has been considered reasonable. To bring the cost down to $50,000, however, 91% of the smokers in the study would have had to undergo a stage shift downward to more treatable lung cancers, the authors wrote.
Among the quitting and former smokers groups, even a 100% stage shift would not have been sufficient to bring the cost of each QALY saved down to $50,000.
"Gains in QALY from screening and treatment did not manifest until the fourth year of follow-up," the authors stated. "There were significant upfront costs for screening, with the largest increase occurring in the first year."
The group also found that screening was most cost-effective when started in individuals aged 55 to 65 years.
Among the limitations, the study did not calculate the benefits, harms, and costs of incidental diagnoses from screening, nor did it calculate costs associated with disability or lost productivity. And future advancements in lung cancer diagnosis and treatment could render the results out of date, the authors stated.
"In summary, we conclude that the hurdles for lung cancer screening with helical CT are set high," they wrote. "In addition to showing substantial reductions in mortality, screening requires high rates of adherence, lower harms, and lower costs per screening test. Given the uncertainty of efficacy, the possibilities of harm, and the high costs associated with screening, direct-to-consumer marketing of helical CT screening is not advisable."
By Eric BarnesAuntMinnie.com staff writer
January 14, 2003
Related Reading
Self-referred screening patients are far less likely to find abnormal results, December 3, 2002
Sputum cytology gives a big boost to CT lung screening, December 2, 2002
Worrisome radiation dose seen in CT lung screening, follow-up, December 23, 2002
Why CT lung cancer screening will (and won't) work, November 11, 2002
Following up incidental findings may do more harm than good, September 5, 2002
CT, x-ray to face off in lung cancer screening megatrial, September 19, 2002
Copyright © 2003 AuntMinnie.com