In western countries, virtual colonoscopy has piqued interest as a means of detecting colon cancer less invasively than endoscopy-based methods such as colonoscopy. It could play that role as well in India, but VC could also have other applications, such as the detection of tuberculosis, according to a group from LTMG Hospital and Medical College in Mumbai.
At the IRIA conference in January in Hyderabad, Dr. Anagha Joshi explained the benefits and advantages of virtual colonoscopy, which is still relatively novel in India. The technique was first described by Vining et al in 1994, but it took nearly six years before CT technology was advanced enough to be able to offer virtual colonoscopy as a commercial product.
There are a number of other techniques available for screening patients for colon cancer, of course, but all have disadvantages. The current gold standard, fiberoptic colonoscopy, is invasive and not well tolerated by patients, and can potentially result in patient morbidity due to a small number of colon perforations that can occur during the procedure.
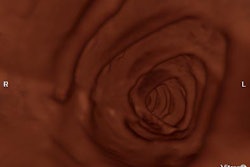
With virtual colonoscopy, the patient undergoes a prep regimen that includes salt and electrolyte mixtures for eliminating stool prior to the exam (dietary fecal tagging, which enables stool to be differentiated from polyps during postprocessing, is a recent alternative to colon cleansing and is described in a 2002 paper in Radiology by Lefere et al. Due to the importance of bowel distension for adequate visualization, the colon is insufflated with room air or CO2. Patients then undergo CT scanning, with images transferred to a 3-D workstation for review, Joshi said.
Currently, multislice CT protocols with thin collimation and overlapping reconstruction are the technique of choice for virtual colonoscopy. The arrival of multislice CT gave a major boost to virtual colonoscopy, enabling the coverage of a large anatomic volume such as the abdomen with collimation as thin as 1 mm in a single breathhold.
Joshi’s group scanned patients with an eight-slice scanner without intravenous or oral contrast media, using 3-mm slices with a collimation of 1.25 mm, a single breathhold of 39 seconds, and a rotation time of 0.5 seconds. The scanner’s effective kV was set to 120, and feed/rotation rate of 5.2 mm. The group also uses 5 mm slices with a collimation of 2.5 mm, single breathhold of 14 seconds, rotation time of 0.5 seconds, an effective mAs of 130, kV of 120, and feed/rotation of 15 mm.
Patients are scanned in a craniocaudal direction with images reconstructed in 1- and 2.5-mm slice thicknesses using a medium-smooth kernel, and displayed using soft-tissue windows. Data are reconstructed and transferred to a dedicated workstation with fly-through endoscopic software.
Virtual colonoscopy data can be visualized in multiple modes, such as surface renderings, volume renderings, and multiplanar reformattings. Annotation, measurement, and other tools are also possible, with data saved as still images or in cine format.
Indications for virtual colonoscopy include the following:
· Screening of patients at high risk for colon cancer.
· Preoperative evaluation of patients with colorectal carcinoma, in particular for localizing lesions.
· Evaluation of patients with failed conventional colonoscopy.
· Follow-up of colorectal surgery patients, to evaluate the post-operative anastomoses via their length, caliber, and feasibility and adequacy of balloon dilatation.
Virtual colonoscopy’s limitations include a lack of sensitivity for detecting polyps smaller than 7 mm. Macari et al demonstrated a sensitivity of 12% for polyps smaller than 5 mm, 70% for polyps 6-9 mm, and 93% for polyps larger than 10 mm. In addition, the technique does not always perform well in detecting flat lesions, and provides no functional information. Finally, VC does not have a therapeutic component: patients must be sent on to conventional colonoscopy if a suspicious polyp is detected, where they must be prepped a second time.
Future developments in virtual colonoscopy include the following:
· The use of MRI rather than CT, which will eliminate concerns about radiation dose.
· The application of computer-aided detection (CAD) protocols to VC data, to help radiologists sort through the large data volumes produced by the exam.
· The development of low-dose scanning protocols, which would make VC more suited for a screening population.
· The development of prepless VC, using electronic fecal tagging methods.
In investigating virtual colonoscopy, Joshi’s group has found that the technique could help detect and diagnose tuberculosis cases, due to the consistent appearance of TB on virtual colonoscopy exams. In a study of 55 patients, nine of them had TB, and a common finding across the cases was a narrowing of the ileocecal lumen with multiple polypoidal lesions.
Virtual colonoscopy’s ability to find extracolonic abnormalities is another important advantage over colonoscopy, giving the technique the ability to evaluate endoluminal, intramural, and pericolonic lesions, as well as other organs likely to be affected by tuberculosis.
“We may be coming to a diagnosis of tuberculosis by just doing virtual colonoscopy, saying that a narrow constricted lumen with multiple nodules is pointing to tuberculosis,” Joshi said.
By Brian Casey
AuntMinnie.com staff writer
March 12, 2004
Related Reading
Group credits 3-D reading for best-ever VC results, October 15, 2003
Virtual colonoscopy not yet an adequate screening tool for colorectal cancer, October 13, 2003
Group favors 3-D primary read in major virtual colonoscopy trial, October 2, 2003
Chest X-ray not necessary to detect active TB in HIV-infected patients, November 7, 2003
In a screening population, virtual colonoscopy finds significant polyps, January 3, 2003
Copyright © 2004 AuntMinnie.com