Many nuclear medicine practices are neglecting to tell patients with diabetes that their medications could affect the image quality of their FDG-PET/CT scans, according to a study published in the June issue of the Journal of the American College of Radiology.
A survey of more than 60 imaging centers found that the majority of facilities failed to provide details on the prescan administration of metformin or short- or long-acting insulin, how long patients should fast, or optimum blood glucose levels. The researchers concluded that results show a "nationwide disconnection" between nuclear medicine practices and their patients' management.
"Advocacy is needed from national organizations to disseminate and implement examination preparation instructions to optimize the diagnostic accuracy of oncologic FDG-PET/CT and to limit unintended harm to patients with diabetes mellitus," wrote the researchers led by Dr. Andrew Kaiser from the department of radiology at the University of Michigan in Ann Arbor.
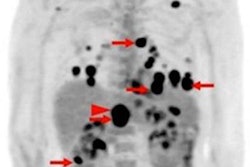
FDG-PET/CT scans for patients with diabetes mellitus can be tricky, given fluctuations in their glucose and insulin levels, which, in turn, can affect image quality. The administration of insulin in close proximity to FDG injection can result in diffusely increased uptake of the radiotracer in skeletal and cardiac muscle, which could obscure malignancies, the authors wrote. Hence, how well patients with diabetes prepare for their FDG-PET/CT scan is extremely important.
Several nuclear medicine and molecular imaging organizations have established guidelines with a number of prerequisites, such as fast time before the exam and discontinuing insulin and possibly metformin before FDG administration. The question is: Do imaging centers provide this information to patients ahead of time?
To find out, Kaiser and colleagues called the scheduling lines of 33 academic and 32 private nuclear medicine practices in five U.S. regions under the pretense of being a family member looking to book an appointment for an FDG-PET/CT scan for a grandmother with diabetes and cancer. Each facility was contacted on three different days for a total of 195 calls.
The researchers also sent emails to program directors of 33 academic institutions with nuclear medicine or nuclear radiology training programs to obtain details on written guidance for patients with diabetes mellitus before undergoing FDG-PET/CT scans for cancer (JACR, June 2019, Vol. 16:6, pp. 804-809).
Kaiser and colleagues found that 179 calls (88%) omitted prescan medication instructions for metformin, 193 conversations (99%) left out guidance for long-acting insulin, and 59 conversations (30%) did not include what to do about short-acting insulin administration.
"When information is provided, it is often heterogeneous, incomplete, and different than national guidelines," the authors noted. For example, 136 calls (70%) correctly recommended that patients withhold use of short-acting insulin before the scan. However, 20 calls (10%) recommended holding short-acting insulin after midnight and 116 conversations (59%) gave a range of durations from four to eight hours. Only 1% of calls correctly gave instruction to hold long-acting insulin after midnight, based on national guidelines.
Somewhat surprisingly, 92 calls (47%) did not provide a method for communicating FDG-PET/CT exam details to patients diabetes, which begged the question whether these facilities follow preparation policies at all.
"There is a nationwide disconnection between local nuclear medicine department policy statements and what is being communicated to patients with respect to the management of diabetes mellitus before FDG-PET/CT," the researchers wrote. "More research is needed to define fasting and medication holding policies and optimal serum glucose thresholds before imaging."