Diffusion-weighted MR imaging (DWI-MRI) can detect injury in children presenting with traumatic brain injury, even if other neurological signs appear normal, according to the results of a new study. The research demonstrates that DWI is predictive of long-term outcomes in pediatric patients.
Early identification of children at high risk for poor six- to 12-month outcomes can be instrumental when deciding to initiate aggressive clinical management of patients with traumatic brain injury. Yet few pediatric studies of DWI have been performed, according to Dr. Nicholas Galloway, lead author of the study published in the October 2008 issue of the Journal of Neurotrauma (Vol. 25:10, pp. 1153-1162). Galloway is a radiation oncologist from Loma Linda University Children's Hospital in Loma Linda, CA.
In addition to eliminating the radiation dose exposure of a CT exam, a DWI-MRI study may reveal diffusion abnormalities hours before CT could detect damaged tissue. DWI also allows for quantification of water mobility by means of determining apparent diffusion coefficient (ADC) values.
ADC values measure the translational, random water motion in the brain as limited by cellular structures and composition. These measurements are useful in detecting diffuse axonal injury, which can lead to memory loss, seizures, cognitive impairment, headaches, and behavior and attention disorders.
Axonal injury or ischemia has been difficult to detect in children because of the relatively high water content of the immature, developing white matter in the pediatric brain. DWI greatly improves the ability to detect the contrast between uninjured and injured immature brain tissue, and it also improves the ability to detect hemorrhagic and nonhemorrhagic lesions, according to the authors.
The patient cohort consisted of 37 children with traumatic brain injury and presumed diffuse axonal injury. The patients had MRI exams performed within 24 hours to 16 days of being admitted to the intensive care unit at Loma Linda. Ten children having MRI exams for different clinical indications were used as the control group. All imaging took place between March 2001 and September 2002.
The average age of the patients with traumatic brain injury was 10.6 years, with a range of 1.5 to 18 years. The average age of the control group was 8.7 years, with a range of 1 to 16 years.
The children were examined by a neurologist or a neurosurgeon and categorized as having mild/moderate (Glasgow Coma Scale 9-15) or severe (Glasgow Coma Scale 3-8) traumatic brain injury. The Pediatric Cerebral Performance Category Scale was used to quantify overall functional and cognitive impairment six to 12 months after injury. The scale's six categories are normal; mild, moderate, or severe disability; persistent vegetative state; and death. The researchers consolidated these categories into two groups: good outcome (normal to mild disability) and poor outcome (moderate to severe disability including vegetative state).
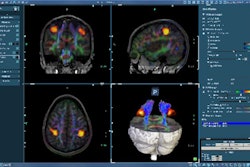
The MRI examinations were performed using a circularly polarized head coil in a conventional 1.5-tesla whole-body scanner (Magnetom Vision, Siemens Healthcare, Malvern, PA). DWI was performed using a single-shot echo-planar technique (TR/TE = 4,000/110 msec, 5 mm thick) in three spatial encoding directions and two b values (500, 1,000 sec/mm²).
Fifteen bilateral regions of interest were manually drawn on ADC maps generated when the images were reviewed. The brain regions were grouped for analysis into categories classified as peripheral gray matter, peripheral white matter, deep white matter, deep gray matter, and posterior fossa. Comparisons between the mean ADC values of the outcome groups and individual regions of interest were evaluated.
The researchers were most interested in determining whether regional ADC values could discriminate between good and poor Pediatric Cerebral Performance Category Scale outcomes in the patients with severe traumatic brain injury. They determined that ADC differences were present only in the peripheral white matter between patients with severe traumatic brain injury who had good outcomes (82.5 ± 3.8) and those who had poor outcomes (72.8 ± 14.4).
Other findings included the following:
- The average total brain ADC values alone had the greatest ability to predict outcome. In this study, these values predicted outcome accurately in 83.8% of the patients, compared to 81% using other clinical variables.
- Deep white matter was more sensitive to long-term tissue alterations.
- Patients with mild/moderate traumatic brain injury and good outcomes had lower peripheral gray matter ADC values (86.7 ± 4.7) than patients with severe traumatic brain injury and good outcomes (94.0 ± 7.0).
The researchers suggest that differences between mechanisms responsible for edema formation between gray and white matter may exist, and that edema formation in gray matter may not be as ominous a predictor of outcome as the presence of edema in white matter.
They further speculate that ongoing cellular remodeling is occurring and is evident only in severely injured patients with good outcomes, with increased ADC reflecting brain repair mechanisms.
"Additional studies correlating our findings with other imaging parameters such as spectroscopy, susceptibility-weighted imaging, and diffusion-tensor imaging will be helpful in objectively quantifying injury severity and will be useful to assess evolution of injury and repair and the effectiveness of treatment," Galloway and colleagues concluded.
By Cynthia Keen
AuntMinnie.com staff writer
November 13, 2008
Related Reading
Diffusion-tensor MRI spots subtle changes after mild traumatic brain imaging, March 31, 2008
Copyright © 2008 AuntMinnie.com