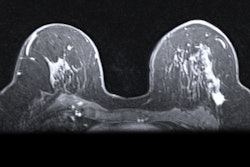
Pretreatment breast MRI can help quantify intratumoral heterogeneity (ITH) and predict pathologic complete response in women undergoing breast cancer treatment, according to research published April 15 in Radiology.
A team led by Yao Huang, PhD, from Chongqing University in China developed a nomogram that combined ITH scoring and clinicopathologic variables. It highlighted the nomogram’s high-achieving performance in predicting pathologic complete response to neoadjuvant chemotherapy and recurrence-free survival.
“Lower nomogram scores were associated with poorer recurrence-free survival,” the Huang team wrote. “Notably, a lower nomogram score was associated with biologic pathways reflecting tumor proliferation.”
Higher ITH levels are tied to poorer treatment response and prognosis in women being treated for breast cancer. Assessing ITH means using invasive methods such as tissue sampling, pathologic evaluation, and genomic sequencing.
Previous research has explored the potential of MRI radiomics in better quantifying ITH while also being noninvasive. However, Huang and colleagues noted that it remains unclear whether this method can predict pathologic complete response to chemotherapy and prognosis in breast cancer patients.
The researchers used pretreatment MRI to quantify ITH in breast cancer. They clustered tumor regions on MRI scans and integrated them with global pixel distribution patterns to calculate ITH scores. From there, the researchers developed a nomogram to predict pathologic complete response to neoadjuvant chemotherapy and recurrence-free survival. They also studied biologic pathways linked to nomogram scores.
Final analysis included retrospective data from 1,448 women with a median age of 49. The women underwent chemotherapy at nine centers between 1988 and 2023.
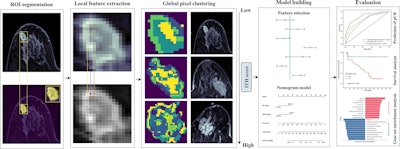 Schematic workflow of the study shows how researchers developed an MRI-based nomogram. First, the team segmented manually delineated tumor regions. Then, they used a 3 × 3-mm sliding window to extract local features. From there, the team performed unsupervised clustering based on local features and generated a schematic diagram to visualize global distribution patterns, calculating the intratumoral heterogeneity (ITH) score. The team evaluated the ITH score and clinicopathologic variables as potential predictors of pathologic complete response. It used independent predictors of complete treatment response to construct a nomogram model. Finally, the researchers validated the performance of the nomogram model in predicting pathologic complete response and recurrence-free survival, as well as its potential biologic meaning.RSNA
Schematic workflow of the study shows how researchers developed an MRI-based nomogram. First, the team segmented manually delineated tumor regions. Then, they used a 3 × 3-mm sliding window to extract local features. From there, the team performed unsupervised clustering based on local features and generated a schematic diagram to visualize global distribution patterns, calculating the intratumoral heterogeneity (ITH) score. The team evaluated the ITH score and clinicopathologic variables as potential predictors of pathologic complete response. It used independent predictors of complete treatment response to construct a nomogram model. Finally, the researchers validated the performance of the nomogram model in predicting pathologic complete response and recurrence-free survival, as well as its potential biologic meaning.RSNA
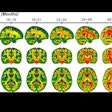
To predict pathologic complete response, the team included 505 women from center A in a training set. They also included women from the remaining centers into three external validation sets: center B (n = 331), centers C to F (n = 107), and center G (n = 384). The survival set meanwhile included women from centers A and H (n = 179) and the genomics set included patients from center I (n = 74).
The ITH score was an independent predictor of complete pathologic response, with an odds ratio of 0.12 (p < 0.001), the researchers found.
In the external validation sets, the nomogram model achieved area under the receiver operating characteristic curve (AUROC) values of 0.82 (center B), 0.81 (centers C to F), and 0.79 (center G), respectively.
Finally, the team reported that a lower nomogram score correlated with poorer recurrence-free survival, with a hazard ratio of 4.04 (p < 0.001). And lower scores were also tied to upregulation of biologic pathways related to tumor proliferation.
“These findings support the biologic significance of the nomogram model including the ITH score, indicating that this model not only can stratify patients by their prognosis but also reflects the biologic characteristics of the tumors,” the study authors wrote.
The authors called for future large-scale prospective studies to validate the clinical value of the nomogram.
The full study can be found here.


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


![Images depict axial MRI scans in a 50-year-old premenopausal female patient with biopsy-proven 12-mm invasive lobular cancer in the lower outer quadrant of the left breast. Upper images are subtracted dynamic contrast-enhanced (DCE) MRI scans from the first and second postcontrast acquisitions. Lower images are ultrafast MRI scans obtained within 24 hours after the DCE study (four consecutive subtracted dynamic frames from time points [T] 6–9). There is marked background parenchymal enhancement (BPE) on the DCE MRI scans. Thus, the known cancer (arrow) is barely visible; it exhibits only slightly stronger enhancement than the normal fibroglandular tissue, which results in low conspicuity. At ultrafast MRI there is less BPE, and still the cancer is barely visible because it starts to enhance simultaneously with the BPE. The conspicuity of the cancer is even reduced compared with the DCE series. Both of the readers missed this cancer on both the DCE and ultrafast MRI scans.](https://img.auntminnie.com/mindful/smg/workspaces/default/uploads/2025/05/2025-05-06-rsna-ultrafast-dce-mri-breast.Gzvq76udFr.jpg?auto=format%2Ccompress&fit=crop&h=167&q=70&w=250)
.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)