Bicuspid Aortic Valve:
Clinical:
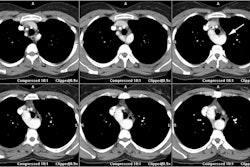
Bicuspid aortic valve is not uncommon (0.5 - 2% of the population), but typically does not present until adulthood. In fact, it is the most common congenital cardiovascular malformation [4,5]. Although the valve may function normally, about 35% of affected patients will develop an abnormally turbulent flow pattern which will lead to valve deformity and calcification. These patients are also at a greatly increased risk for infective endocarditis [5]. Slowly evolving aortic regurgitation may result if the valve leaflets fail to close normally.The incidence is higher in Turner's syndrome, coarctation of the aorta and VSD [3]. Approximately 26% of patients with BAV have aortic coarctation, but 50-70% of patients with coarctation have BAV [4]. Other defects associated with BAV include patent ductus arteriosus, supravalvular aortic stenosis, WIlliams syndrome, subvalvular aortic stenosis, Shone syndrome, and coronary artery anomalies [4]. Affected patients usually have three sinuses of Valsalva, but there is loss of the normal pattern of symmetry. The non-coronary sinus becomes larger and extends more posterior and inferiorly [2].
The most common complication of BAV is aortic stenosis [4]. Stenosis occurs earlier if the aortic cusps are asymmetric or fused in the anteroposterior position (fusion of the right coronary and noncoronary cusps) [4]. Aortic regurge occurs more commonly in younger patients than does aortic stenosis and is caused by prolapse of a larger cusp, fibrotic retraction of the cusps, and aneurysmal dilatation of the aortic root and valve annulus [4]. Patients with BAV are also at an increased risk for aortic dilatation, aneurysm, and dissection [4,5]. Aortic dissection occurs 5-10 times more frequently in patients with BAV than in those with a normal aortic valve [4]. Because of this fact, guidelines suggest intervention for an asymptomatic ascending aortic aneurysm in patients with BAV when the aneurysm diameter reaches 4 or 5 cm, instead of the 5.5 cm recommendation for the general public [5].
X-ray:
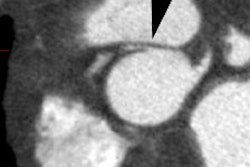
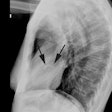
Most commonly the two cusps are unequal in size because of congenital fusion of one of the valve commissures [5]. The most common pattern of fusion is of the left and right cusps (this pattern is associated with valvular stenosis) [5]. Valves in which the right and noncoronary cusps are fused appear to be affected by stenosis and reguritation with roughly equal frequency [5]. Calcification in the BAV is largely confined to the base of the conjoined cusp and the raphe [4]. A "ring calcification" with or without a calcified central raphe usually occurs by age 30 years and is best appreciated on the lateral view.If aortic stenosis is present, there will be evidence of post-stenotic dilatation of the ascending aorta on the frontal CXR.
REFERENCES:
(1) J Thorac Imag, 95, 10: p.1-25
(2) Radiologic Clinics of North America 1999; Lipton MJ, Coulden R.
Valvular heart disease. 37(2): 319-339
(3) AJR 2008; Takaki MTTT, et al. Nonatherosclerotic cardiovascular
findings on MDCT coronary angiography: a selection of abnormalities.
190: 934-946
(4) AJR 2012; Ko SM, et al. Bicuspid
aortic valve:
spectrum of imaging findings at cardiac MDCT and cardiovascular MRI.
198: 89-97
(5) Radiographics 2012; Bennett CJ, et al. CT and MR imaging of the aortic valve: radiologic-pathologic correlation. 32: 1399-1420