Ventricular Septal Defect:
View cases of VSD
Clinical:
Other than for a bicuspid aortic valve, VSD is the most common type of congenital heart disease accounting for about 25% of cases. The majority of patients are asymptomatic, but patients may present with CHF in infancy if there is a large defect, systolic murmur, or bacterial endocarditis. Small VSD's may go undetected until adulthood. As with ASD's if long standing VSD's can lead to Eisenmenger's physiology. Eisenmenger's represents the development of high pulmonary vascular resistance after many years of increased pulmonary blood flow (ASD/VSD/PDA). The increased flow results in reactive muscular hypertrophy and endothelial thickening/sclerosis of microscopic pulmonary vessels which eventually leads to their obliteration. This results in elevated pulmonary arterial and right ventricular pressures. If the pressure becomes high enough, there will be reversal of the shunt (ie: R to L). On CXR Eisenmenger's is characterized by marked dilatation of the central pulmonary arteries and pruning of peripheral arteries. There is also RV enlargement and no redistribution of flow to the pulmonary veins (normal venous pressure). After the development of Eisenmengers syndrome, clsoing the VSD is contraindicated as right heart failure will result [3]. Types of VSD's include:
1- Perimembranous: Most common (80%). The defect involves the membranous septum and a small portion of adjacent muscular septum, usually posterior and inferior to crista supraventricularis. These defects are typically larger than muscular septum defects and are more likely to produce symptoms. The LV usually communicates with the RV, but can communicate with the RA. There may be an associated small aneurysm of the membranous septum. The defect lies along the LV outflow tract immediately under the aortic valve. The septal leaflet of the tricuspid valve can appose over the defect. About 25% will close spontaneously.
2- Muscular: (10-20%) Defect is in the muscular portion of the septum and is usually obliterated during systole. About 65% will close spontaneously.
3- Posterior or Inlet: Defect is adjacent to septal and anterior leaflets of the mitral valve. Associated with endocardial cushion defect.
4- Conal: (Supracrista) Defect is located superior to the crista supraventricularis- along right ventricular outflow tract and immediately below the right cusp of the aortic valve. The right aortic valve cusp may herniate into the VSD with resultant aortic insufficiency. The prolapsed cusp can partially or completely seal the defect.
Syndromes associated with an increased incidence of VSD include: Down's syndrome, Holt-Oram, Absent radius with ulnar bowing, and Hypoplastic/Absent thumb (Less commonly may see tri-phalangeal thumb). Cardiac anomalies associated with an increased incidence of VSD include: Tetrology, Transposition, Truncus, Coarctation/Interruption of the aortic arch, ASD/PDA, and AP window.
Most small VSD's will close spontaneously by age 5 years (about 30-60% of VSD's). Pulmonary artery banding may be performed if definitive repair is not possible. This is an attempt to decrease the risk of developing pulmonary arterial HTN by decreasing the amount of systemic to pulmonic shunting.
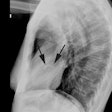
X-ray:
With small VSD's the CXR may be normal. Larger VSD's will demonstrate shunt vascularity, LAE (due to increased return to this chamber), RVE (blood tends to flow through RV into pulmonary outflow tract, initially resulting in enlarged pulmonary trunk with normal appearing RV), PA enlargement. The RA is excluded from the shunt, and the aorta also has a normal appearance. CHF soon after birth is associated with large VSD's.
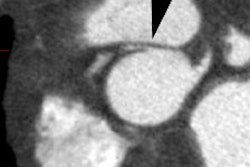
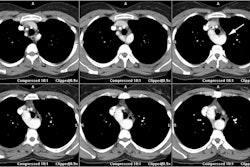
On MR imaging, membranous ventricular septal defects are identified by the absence of signal in the superior most aspect of the interventricular septum. However, it is important to remember that a portion of the membranous septum may not be identified normally- increased confidence in the diagnosis is obtained by identifying the defect on two contiguous images or two separate planes. Small muscular VSD's are more difficult to identify on spin echo images, but moderate to large lesions are easily see on SE. Cine gradient-echo images will demonstrate the signal void associated with the shunted blood and aid in the identification of small lesions.
REFERENCES:
(1) Pediatric Clinics of North America 1999; Driscoll DJ. Left-to-right shunt lesions.
46(2): 355-368
(2) Radiographics 2007; Leschka S, et al. Pre- and postoperative evaluation of congenital heart disease in children and adults with 64-section CT. 27: 829-846
(3) Radiology 2008; Gaca AM, et al. Repair of congenital heart disease: a primer- part 2. 248: 44-60