Myocarditis:
Clinical:
Myocardial inflammation (myocarditis) can be secondary to a
number
of etiologies including infection (typically viral or HIV),
cardiotoxic
agents (drugs, chemotherapy- anthracyclines), autoimmune (SLE), or
post-transplant
rejection [7]. The most common viral agents are coxsackie B virus
(accounts
for 50% of cases [7]), noncoxsackie enterovirus, herpes virus 6,
adenovirus, and parvovirus B19 [6,7]. The incidence of myocarditis
in
HIV patients is reported to be between 6-52% and no specific
pathogen
is found in more than 80% of cases [10]. It is a lymphocytic
myocarditis in about half of the cases [10]. Common pathogens
indentified in HIV myocarditis include toxoplasma gondii,
mycobactrium
tuberculosis, and cryptococcus neoformans [10].
The level of troponin I is more
often elevated than that of CK-MB in patients with myocarditis
[8]. For
viral myocarditis,
spontaneous recovery within a few weeks to months is common [3,4].
However, chronic myocarditis (dilated cardiomyopathy) occurs in
10-21%
of cases [3,11]. Sudden cardiac death can occur in up to 12% of
young
adults [6].
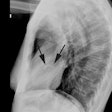
X-ray:
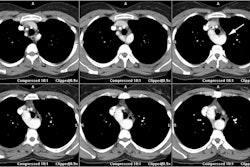
MR: The diagnosis of myocarditis is made on the basis of two of
three "Lake Louise" criteria: 1- regional or global signal
intensity increase on T2 images; 2- increased global myocardial
early gadolinium enhancement ratio (EGEr ≥4.0); 3- at least one
focal, nonischemic lesion at inversion-recovery late gadolinium
enhancement imaging [12].
Focal or global areas of increased signal can be seen within the
myocardium on T2 images [7]. Cine balanced steady-state free
precession
(SSFP) sequences (which yield high contrast between blood and
myocardium) can also be used to detect acute inflammation [9].
Owing to
the T1 component of the signal, SSFP MRI sequences following
contrast
administration correlate well with areas of enhancement on delayed
contrast imaging [9]. In areas of myocardial inflammation, the
increased T2 relaxation time- due to edema- combined with the
decrease
in T1 relaxation after contrast administration allows detection of
myocardial abnormalities [9].
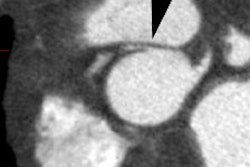
Delayed myocardial enhancement can be seen
in 24-88% of cases of acute viral myocarditis [7]. With acute
myocarditis, delayed hyperenhancement is generally scattered,
nodular
and
subepicardial (or midmyocardial as opposed to vascular disease
that
produces
subendocardial abnormalities), without respect for vascular
territories, and often with an inferolateral/lateral and apical
distribution [1,2,4,8]. The changes may be subtle and focal
acutely,
becoming more diffuse over the next 10 days [1].
Although subepicardial enhancement is seen in the majority of
cases,
focal transmural areas of enhancement can occur in severe cases
[5]. In
myocarditis, myocardial damage is more diffuse than damage due
to
infarction.
Islands
of
necrotic
cells
are scattered throughout the
focus
of acute myocarditis [2]. Therefore, contrast enhancement in
acute myocarditis may not be as intense as in myocardial
infarction [2]. With herpes 6 infection, it has been
suggested
that the septum is primarily involved, and that with parvovirus
19,
there is a predilection for the inferolateral wall [7].
During healing, inflammatory cells infiltrate
the
myocardial regions of myocarditis, and eventually
necrotic
myocytes are replaced by areas of fibrous tissue and
delayed contrast enhancement can persist in the
chronic
phase [2]. The area of myocarditis diminishes in size as it is
replaced
by scar and this can explain the observation that
contrast
enhancement typically decreases over time [2].
REFERENCES:
(1) AJR 2007; Lim RP, et al. Non-ischemic causes of delayed myocardial hyperenhancement on MRI. 188: 1675-1681
(2) Radiographics 2006; Vogel-Claussen J, et al. Delayed enhancement MR imaging: utility in myocardial assessement. 26: 795-810
(3) Radiology 2008; Gutberlet M, et al. Suspected chronic myocarditis at cardiac MR: diagnostic accuracy and association with immunohistologically detected inflammation and viral persistence. 246: 401-409
(4) AJR 2009; Goitein O, et al. Acute myocarditis: noninvasive evaluation with cardiac MRI and transthoracic echocardiography. 192: 254-258
(5) Radiographics 2009; Cummings KW, et al. A pattern-based approach to assessment of delayed enhancement in nonischemic cardiomyopathy at MR imaging. 29: 89-103
(6) Radiographics 2009; Sparrow PJ, et al. CT and MR imaging
findings in patients with acquired heart disease at risk for
sudden
cardiac death. 29: 805-823
(7) AJR 2011; Hoey ETD, et al. Cardiovascular MRI for assessment
of
infectious and inflammatory conditions of the heart. 197: 103-112
(8) Radiographics 2011; James OG, et al.
Utility of FDG PET/CT in inflammatory cardiovascular disease.
31:
1271-1286
(9) AJR 2011; Deux JF, et al. Acute
myocarditis
diagnostic value of contrast-enhanced cine steady-state free
precession
MRI sequences. 197: 1081-1087
(10) AJR 2012; Nakazono T, et al.
HIV-related cardiac complications:
CT and MRI findings. 198: 364-369
(11) Radiology 2012; O'Donnell DH, et al. Cardiac MR imaging of
nonischemic
cardiomyopathies: imaging protocols and spectra of appearances.
262:
403-422
(12) Radiology 2014; Acute myocarditis: multiparametric cardiac
MR imaging. 273: 383-392