Total U.S. healthcare system costs for initial cancer screenings in 2021 were $43.2 billion, according to a report published August 5 in Annals of Internal Medicine.
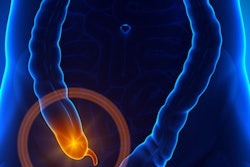
Researchers at the U.S. National Cancer Institute (NCI) found that colorectal cancer represented approximately 64% of the total cost, with colonoscopies making up about 55% of the total. The total cost is less than the reported annual cost of cancer treatment in the first 12 months after diagnosis, the group noted.
“Identification of cancer screening costs and their drivers is critical to help inform policy and develop programmatic priorities, particularly for enhancing access to recommended cancer screening services,” wrote lead author Michael T. Halpern, MD, PhD, of the NCI’s Division of Cancer Control and Population Sciences in Bethesda, MD.
More than two million new cancer cases and more than 611,000 cancer deaths are projected to occur in the U.S. in 2024, according to the authors. While cancer screening may decrease cancer mortality and treatment costs, the cost of screening in the U.S. is unknown, they added.
To address the knowledge gap, the group analyzed data made available in 2021 from the U.S. Centers for Disease Control and Prevention in its National Health Interview Survey (NHIS). NHIS data are collected through personal household interviews.
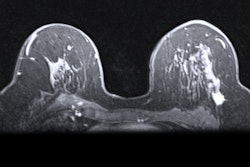
The study considered breast, cervical, colorectal, and lung cancer screening, as well as prostate cancer screening among men aged 55 to 69 years. For breast cancer, the study considered screening among women aged 40 to 49 years old only by mammography. Types of colorectal cancer (CRC) screening methods included colonoscopy, sigmoidoscopy, CT colonography, fecal immunochemical testing (FIT), and Cologuard.
According to the results, mammography (32.8 million) and cervical cancer screenings (33 million) accounted for the largest total number of tests. An estimated 22.3 million CRC screening tests were performed, mainly comprising FIT (9.8 million) and colonoscopy (9.2 million).
Of the estimated $43 billion total, the largest component was screening colonoscopy, which accounted for $23.7 billion, or approximately 55% of the total, the researchers reported. All other CRC screening tests combined accounted for an additional $3.8 billion.
Breast cancer screening accounted for 20.4% of the total ($8.8 billion), and cervical cancer screening accounted for 12.8% ($5.5 billion), while lung cancer screening accounted for approximately 1.5% ($656 million) and prostate cancer screening (PSA tests) accounted for 1.6% ($702 million).
In addition, people with private insurance accounted for more than 88% of all screening costs; Medicare beneficiaries accounted for 8.5%; and Medicaid beneficiaries, those with coverage from another government program, and uninsured persons accounted for 3.2%.
The authors noted limitations, namely that the estimates are only for the number and medical care cost of initial cancer screening tests and do not include costs for follow-up for abnormal initial screening results, although these are critical components of the screening process.
Ultimately, they wrote that screening for breast, cervical, colorectal, and lung cancer has generally been reported to be cost-effective in the U.S. and that colorectal cancer screening may be cost-saving in certain scenarios. The cost-effectiveness of prostate cancer screening is less clear, they noted.
“This study provides previously unavailable estimates for the annual medical care cost of cancer screening in the United States,” the group concluded.
The full study is available here.