The presence of coronary artery calcium (CAC) at CT can improve risk assessment in patients with low LDL cholesterol -- even in those considered to be at low risk of cardiac events, according to a new study in the Journal of the American College of Cardiology.
Researchers from Brigham and Women's Hospital and other centers undertook the study to determine if traditional risk factors were adequate for patients with low LDL cholesterol (LDL-C) -- or if new risk factors could be identified in this population that could be used to pinpoint those who might benefit from statin therapy.
The study, based on patients with low LDL-C levels who participated in the Multi-Ethnic Study of Atherosclerosis (MESA), found CAC to be a "powerful risk marker" for cardiac events that increased the risk of other factors including older age, male sex, hypertension, diabetes, and low HDL cholesterol.
The results show that "even after accounting for all relevant traditional clinical risk factors (and even after considering populations with multiple coexisting risk factors), the presence and burden of CAC can be used to further enhance risk assessment, whereas its absence is associated with a very low event rate," wrote Dr. Ron Blankstein, from Brigham and Women's Hospital, and colleagues at several other centers, in an article published online (JACC, July 11, 2011).
The study examined 3,714 individuals (66% of MESA participants) with LDL-C levels < 130 mg/dl, calculating unadjusted and adjusted hazard ratios to evaluate the association of traditional risk factors and biomarkers with coronary heart disease (CHD) events.
"There are several important reasons to study populations with low LDL-C," the group wrote. "First, although many of the risk factors identified in our study (i.e., hypertension, low HDL-C) have been extensively studied, the relevance of these risk factors among persons with baseline low LDL-C is less established."
In addition, while several studies have sought to assess different risk stratification methods that would add value beyond that of low LDL-C levels, "they have not assessed whether it is possible to distinguish high-risk from low-risk patients from among patients who already have very low LDL-C levels," Blankstein and colleagues wrote.
The study aimed to determine if subclinical atherosclerosis markers provided additional information beyond traditional risk factors in patients with low LDL-C. Coronary artery calcium and carotid intima-media thickness were each separately added to the multivariable model.
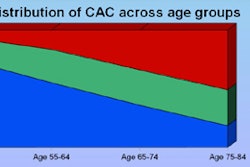
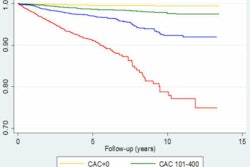
Over a median 5.4 years of follow-up, the researchers observed 120 (3.2%) cardiac events in the study population. Unadjusted analysis pointed to age, male sex, hypertension, diabetes mellitus, low HDL-C, and high triglycerides. Of the imaging-based risk markers, the presence of any CAC was the most powerful predictor of cardiac events, with a hazard ratio of 13.5, while increased carotid intima-media thickness also predicted CHD events.
Among low LDL-C participants, aside from age and sex, the three independent clinical predictors that emerged as significant risk factors were hypertension, diabetes, and low HDL-C. The hazard ratio for individuals with one risk factor was 2.79, for two risk factors was 5.15, and for three risk factors was 9.97, the group reported.
The researchers then calculated hazard ratios after adding in CAC scores to the traditional risk factors, and also after adding in Framingham risk scores. They found hazard ratios for this multivariate analysis as follows:
Hazard ratios by CAC score
|
What's more, adding CAC scores to the multivariate analysis increased the area under the receiver operator characteristics (ROC) curve from 0.815 to 0.857 (p < 0.001). Meanwhile, the relationship between low carotid intimal-medial thickness and cardiac events was much weaker.
"Regardless of the number of risk factors present, the presence of CAC was found to consistently be associated with higher CHD events," Blankstein and colleagues wrote.
The study was limited by the low rate of cardiac events in the study population, and by the fact that screening subjects knew their CAC scores, potentially leading them to seek more treatment, according to the authors.
"Our findings support the need for comprehensive risk assessment in patients with low LDL-C. Specifically, low HDL-C and the presence of hypertension or diabetes should alert clinicians of patients who might benefit from preventive measures," they wrote.
Systematic screening for CAC can't be recommended by these study findings alone, and in any case is unlikely to be cost-effective, according to the authors. But for patients in whom such information would result in a change in medical therapy, evaluating CAC might be reasonable.
"These results may serve as a basis for deciding which patients with low LDL-C may be considered for more aggressive therapies," they wrote.
On the other hand, the absence of coronary calcification "can be used as a reassurance and may signal that there is no need to intensify current therapies, or the threshold for LDL-C-lowering therapy can be higher than if there was advanced subclinical atherosclerosis," the group wrote. "In particular, middle-aged persons who have two or fewer risk factors and no coronary calcification have an extremely low event rate over a six-year follow-up."