
VIENNA - Most radiologists don't deal much with dental imaging -- but that doesn't mean they shouldn't be aware of what to look out for or know about the difference between dental MRI and cone-beam CT (CBCT), expert speakers believe.
In a session on Sunday, ECR delegates had a chance to learn all about dental imaging. When imaging the head and neck region with CT or MRI, teeth are always present, according to chairperson Dr. Julia Frühwald-Pallamar, an assistant professor in the radiology department at the Medical University of Vienna in Austria. On scans performed for other indications, radiolucent or radiopaque lesions of the jaw can be encountered, and familiarity with typical dental conditions is necessary to decide on the right therapy for patients.
The ins and outs of dental MRI
"Obviously, dental MRI is not yet applied in daily routine imaging of teeth or the periodontal apparatus," said Dr. Stefan Rohde, from the Klinik für Radiologie und Neuroradiologie at Klinikum Dortmund in Germany. "However, inflammatory periodontal disease is the major cause of tooth loss in adults, the second most frequent pathology of the oral cavity, and an important cause of disability."
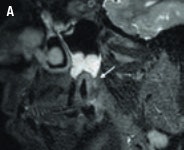
 High-resolution (3-tesla) MRI of a patient with an inflammatory endoperiodontal lesion at tooth 017 (arrow). Sagittal T2-weighted space (A), T1-weighted plus gadolinium (B). Images courtesy of Dr. Stefan Rohde.
High-resolution (3-tesla) MRI of a patient with an inflammatory endoperiodontal lesion at tooth 017 (arrow). Sagittal T2-weighted space (A), T1-weighted plus gadolinium (B). Images courtesy of Dr. Stefan Rohde.Imaging in these patients is usually performed with 2D panoramic radiography, CT, or CBCT. However, MRI may represent a complementary imaging technique to visualize particular pathological processes, especially inflammatory disease of the periodontal space, or teeth vascularization after trauma, he said. His presentation focused on the potential of high-resolution MRI in this new field and compared it with CT and CBCT.
Dentists may make special use of MRI in difficult situations, for example when conventional imaging fails to detect inflammatory or neoplastic processes at an early stage, because visualization is only possible when resorption of the alveolar bone has already started. In addition, MRI offers an alternative technique especially in younger patients and children to avoid radiation exposure, he added.

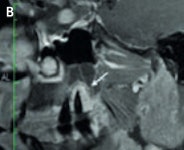
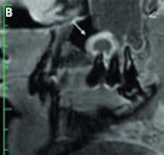 T2-weighted (A) and contrast-enhanced T1-weighted images (B) of a patient with a periapical granuloma at tooth 015 (arrow) and odontogenic sinusitis in the maxillary sinus (open arrow). Images courtesy of Dr. Stefan Rohde.
T2-weighted (A) and contrast-enhanced T1-weighted images (B) of a patient with a periapical granuloma at tooth 015 (arrow) and odontogenic sinusitis in the maxillary sinus (open arrow). Images courtesy of Dr. Stefan Rohde."MRI of the dental apparatus is technically challenging as the bony structures of the mandible and teeth give only little or no MR signal," Rohde said. "Another concern is the problem of air content and metal artifacts in the oral cavity that limit the use of MRI in this special setting. As a principal finding of our experiments, MRI proved to be superior to MDCT [multidetector-row CT] and to CBCT in visualizing periodontal structures like the periodontal space and the adjacent lamina dura. Surprisingly, even cortical and trabecular bone were displayed better with MRI than with MDCT and CBCT. Therefore, I believe that MRI could become an important complementary imaging source of the jaw and teeth apparatus in pathologies of tissue investing and supporting the teeth."

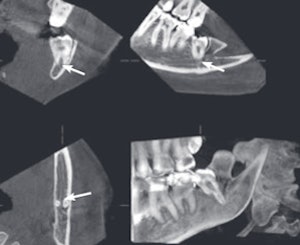
 An example of cone-beam CT. In this instance, the lower left third molar (d. 38) was imaged after panoramic radiograph with CBCT. The arrows mark the mandibular canal. Images courtesy of Dr. Anni Suomalainen.
An example of cone-beam CT. In this instance, the lower left third molar (d. 38) was imaged after panoramic radiograph with CBCT. The arrows mark the mandibular canal. Images courtesy of Dr. Anni Suomalainen.
MRI could be useful to better characterize soft-tissue processes, or detecting inflammatory or neoplastic pathologies at an early stage, he noted. Moreover, dynamic high-resolution MRI with a contrast agent might be an interesting option to visualize teeth vascularization after trauma, or to monitor inflammatory changes under therapy, such as in patients with periodontal disease.
"Delegates should become aware of the fact that MRI in odontology is technically feasible and might be an alternative imaging technique in patients with inflammatory or neoplastic lesions, periapical lesions, or after teeth trauma," Rohde said.
What to know about CBCT
The CBCT technique is well-known among dentists and oral radiologists, but it's not so well-known among general radiologists. It's very important that general radiologists are familiar with this technique and that they know the indications for its use, according to Dr. Anni Suomalainen, from the radiology department at Helsinki University Central Hospital in Finland.
CBCT is a radiographic imaging method that allows accurate 3D imaging of hard tissues. During a CBCT scan, the scanner rotates around the patient's head (180° to 360°), obtaining multiple sequential planar projection images by a 2D detector. The scanning software collects the data, which are then processed to create a volumetric dataset with isotopic voxels with varying field-of-view.
The pitfalls with CBCT are artifacts, which are either physics-based, patient-related, or cone-beam-related. For example, metal objects in the scan field can cause severe streaking artifacts, and patient motion during the exposure can lead to lack of sharpness in reconstructed images.
"Low-dose CBCT examinations with high quality will be further developed, as well as artifact-reduction algorithms," Suomalainen said. "In addition, the use of CBCT devices in other fields of medicine will be increased, and with increasing research results, its use will be more evidence-based."
Originally published in ECR Today on 9 March 2014.
Copyright © 2014 European Society of Radiology



















