Bronchoscopy guided by conebeam CT (CBCT) and "augmented" fluoroscopy can yield 90% accuracy in biopsying peripheral lung lesions, according to research published in the October issue of the Journal of Bronchology & Interventional Pulmonology.
Researchers from Radboud University Medical Center in the Netherlands and Philips Healthcare performed an observational study on over 200 patients who received a CBCT-guided navigation bronchoscopy that included a CBCT image overlay on fluoroscopy imaging. Although there was an initial learning curve and imaging protocols needed to be modified and tailored to the procedure, the image-guided endobronchial lung biopsy method eventually yielded 90% accuracy -- and much lower effective radiation dose for patients and staff.
"Navigation bronchoscopy using CBCT and [augmented fluoroscopy] imaging as a sole technique for both navigation and sampling is a (relatively) safe and accurate procedure for diagnosis of small peripheral pulmonary lesions," wrote first author Roel Verhoeven of Radboud and colleagues.
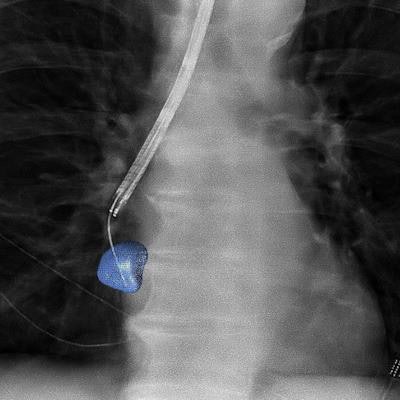
CBCT can acquire intraprocedural 3D information, a valuable benefit for positioning of biopsy tools. The modality can also enable what the researchers called "augmented fluoroscopy," a technique that provides a navigation pathway and lesion position as an overlay on 2D fluoroscopic imaging, according to the researchers.
"With this combination of features, CBCT has the potential to meticulously help guide the endoscopist during the different aspects of the procedure," they wrote.
As this approach to guiding endobronchial diagnosis of challenging peripheral pulmonary lesions relies on augmented fluoroscopy and repeated CBCT scans for navigation and confirmation of positioning, the researchers hypothesized that the learning curve -- and necessary protocol and system modifications -- associated with this method would result in significant variation of radiation exposure to both patient and staff. They therefore sought to assess exposure and procedural diagnostic accuracy over time in a prospective evaluation of 238 consecutive patients at Radboud between December 2017 and June 2020.
After exclusion criteria were applied, 100 cases were available for radiation dose analysis and 208 patients with a total of 248 lesions were included in the accuracy analysis. Of the 208 patients, a primary CBCT and augmented fluoroscopy approach was performed in 150 cases; a primary electromagnetic navigation approach was utilized in the remaining 58 cases.
The researchers observed significant improvements in dose-area product (DAP) and accuracy over time due to factors such as gaining more experience with using the method, fine-tuning of CBCT and fluoroscopy imaging protocols for the procedure, and replacing their CBCT system with an Azurion angiography system (Philips).
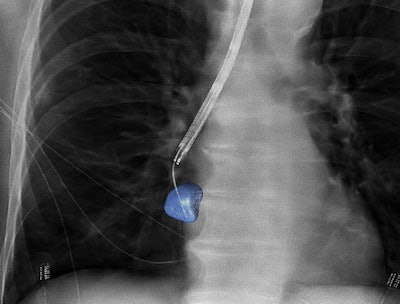 3D image guidance provided via conebeam CT and "augmented" fluoroscopy can improve accuracy in biopsies of peripheral lung lesions. CBCT Image courtesy of Philips Healthcare.
3D image guidance provided via conebeam CT and "augmented" fluoroscopy can improve accuracy in biopsies of peripheral lung lesions. CBCT Image courtesy of Philips Healthcare.
| Impact of CBCT and augmented fluoroscopy guidance on accuracy and radiation dose of bronchoscopy procedures | ||
| Initial experience with CBCT guidance and augmented fluoroscopy in bronchoscopy guidance | After years of using CBCT guidance and augmented fluoroscopy in bronchoscopy guidance | |
| Average procedural DAP | 47.5 Gy·cm2 | 25.4 Gy·cm2 |
| Average estimated effective dose | 14.3 millisieverts | 5.8 millisieverts |
| Accuracy | 72% | 90% |
The lowered radiation dose was primarily attributable to the implementation of lower-dose fluoroscopy protocols, which led to drop in average fluoroscopy DAP from 19 Gy·cm2 to 2.2 Gy·cm2. This dose reduction was achieved despite an increase in average total fluoroscopy time from 9.9 minutes to an average of 15.6 minutes.
"Considering the accuracy of the CBCT-guided navigation bronchoscopy, the procedural radiation burden for the patient when related to other procedures, and the associated cost of some of the additional navigation guidance modalities, one needs to individually assess if having multiple navigation guidance modalities remains worthwhile," the authors wrote. "On the basis of our experience, the added value of CBCT and [augmented fluoroscopy] when compared with other non–real-time navigation technology such as [electromagnetic navigation] is greatest in lesions needing more meticulous positioning."