An AI model shows promise for identifying on x-ray difficult-to-detect physeal fractures in children, a team at the Children’s Hospital of Philadelphia has reported.
The model was developed on 2,103 x-rays comprised of anteroposterior and lateral views from 1,082 patients (mean age, 10) and achieved an accuracy of 84% at the task, noted lead author Nathan Chaclas, MD, an orthopedic surgeon, and colleagues.
“These results suggest that our model may be most beneficial as a decision-support tool in urgent care and emergency room settings where physeal fractures necessitate an orthopedic referral and nonphyseal fractures may not,” the group wrote. The study was published November 8 in the Journal of the Pediatric Orthopaedic Society of North America.
Distal radial fractures occur in the radius bone near the wrist, and often involve the physis. Typically caused by falls, they are among the most common pediatric injuries. However, they can be challenging to diagnose, with misdiagnosis rates reported as high as 46%, the researchers noted.
They wrote that this is because patients frequently do not present to a pediatric orthopedic surgeons or musculoskeletal radiologists initially, but to urgent care and emergency room physicians. Thus, the group aimed to develop an AI model that could help in these settings.
The researchers first split data from 2,103 x-rays into training, validation, and test sets, with a ratio of 60:20:20. They trained a particularly powerful family of convolutional neural networks (CNNs) called EfficientNet. Developed by scientists at Google AI in 2019, these models range from EfficientNet-B0 to EfficientNet-B7 and increase in complexity as they advance.
After training, they compared the performance of the EfficientNet models from B0 to B7, and selected the best model based on the highest F1 score. The F1-score is a measure of a model’s accuracy that considers both precision and recall, and provides a single score that balances the two. A score closer to 1 indicates better overall performance.
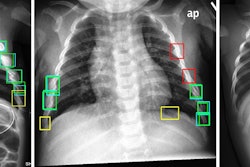
 Grad-CAM heatmap of the EfficientNet-B2 model for a sample radiograph.Journal of the Pediatric Orthopaedic Society of North America
Grad-CAM heatmap of the EfficientNet-B2 model for a sample radiograph.Journal of the Pediatric Orthopaedic Society of North America
In addition, to interpret the model's predictions, the researchers used Grad-CAM, a technique that visualizes the regions of the radiographs that the model learned to focus on for classification.
“Fine-tuning an EfficientNet model can achieve high accuracy in identifying physeal fractures. Further, Grad-CAM provides interpretability and transparency for the model's predictions, highlighting regions of interest and potential sources of error,” the group wrote.
Improving diagnostic accuracy for physeal fractures in children could have a significant clinical impact, the researchers noted. Misdiagnosis can lead to growth arrest and deformities that require complex surgeries later in life, such as physeal bar resection, corrective osteotomies, or epiphysiodesis, all of which carry their own risks and costs, the researchers wrote.
Moreover, work in this area to date has focused on demonstrating the use of various AI models to detect distal radial fractures in adults, which may not perform similarly in children, they noted.
“Future work should include expanding the dataset with more diverse and balanced samples and testing the model on different views and fracture patterns,” the researchers concluded.
The full study is available here.