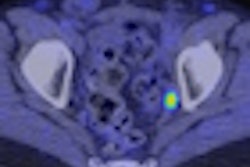
Dutch researchers have found 11C-choline PET imaging to be more accurate than MRI or CT in staging of lymph node involvement in prostate cancer; meanwhile, a new U.S. database analysis says that younger prostate cancer patients shouldn’t be steered away from radiation therapy merely because of their age.
A prospective study of 67 patients at the Groningen University Hospital in Groningen pegged the sensitivity of 11C-choline PET for staging of metastatic lymph node disease at 80% and the specificity at 96%, for an overall accuracy of 93%. These figures, found in the latest issue of the Journal of Nuclear Medicine, represent the first published assessment of 11C-choline PET’s performance for this application, according to the authors.
For this study, 67 patients underwent imaging on an ECAT 951/31 or an ECAT Exact HR+ PET scanner (Siemens Medical Solutions, Erlangen, Germany; CTI Molecular Imaging, Knoxville, TN) after the injection of 400 MBq of 11C-choline.
In contrast, the combined accuracy of MRI and CT among study patients was 86%, derived from a specificity of 98% and sensitivity of only 47%. While the study wasn’t designed to compare these anatomical approaches to the PET technique, the findings were consistent with other investigations of MRI and CT for lymph node staging.
"Conventional imaging techniques such as CT and MRI have been shown to have a low sensitivity in determination of tumor involvement of pelvic lymph nodes, because nodal involvement is not always correlated with enlargement," the authors noted (JNM, March 2003, Vol. 44:3, pp. 331-335).
CT’s sensitivity in detecting nodal metastases has been reported from 25% to 70%, and neither MRI nor lymphangiography has demonstrated higher sensitivity, the authors stated.
"Recent improvements with contrast-enhanced MRI and rapid imaging sequences, as well as with CT using lower cutoff values for pathologic lymph nodes combined with fine-needle aspiration, have led to an increased sensitivity of 75%-78%," the researchers wrote. "Still, for accurate nodal staging, a histopathologic examination of pelvic lymph nodes dissected by pelvic lymphadenectomy is needed."
Laparoscopic or open surgical lymphadenectomy is the gold standard for pelvic node staging, but also involves a reported morbidity of 5%-7%. "Therefore, an accurate noninvasive method for pelvic lymph node staging in prostate cancer would be welcomed," wrote the authors, who also noted that determining tumor involvement in the regional lymph nodes is "of key importance for the proper planning of treatment."
18F-FDG PET has also been examined as a means for lymph node staging, the authors added, but "the urinary radioactivity seen with 18F-FDG has practical implications such as bladder irrigation for the proper use of this technique."
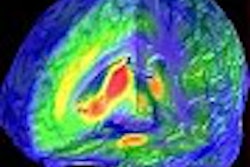
Age and disease-free survival not linked
In another new study with implications for prostate cancer therapy, researchers have found that a patient’s age and their chance of disease-free survival after radiotherapy are not related, and therefore, age "may not be a valid factor in choosing between primary treatment options."
The findings, which were also reported at the 2002 meeting of the American Society for Therapeutic Radiology and Oncology (ASTRO), reflect an analysis of records from 1,018 patients treated at military and VA healthcare facilities from around the advent of prostate-specific antigen (PSA) testing in 1988 through the year 2000. The U.S. Department of Defense Center for Prostate Disease Research funded the study.
"The effect of age at presentation (on prognosis) is generally a subject of some unease, because, in the pre-PSA era, patients presenting with CaP at a young age were considered to be subject to lesions of a more virulent biology, with attendant poorer outcomes," the authors noted, adding that "young age" is also "subject to considerable interpretation" (International Journal of Radiation Oncology, Biology, and Physics, March 15, 2003, Vol. 55:4, pp. 964-969).
The researchers looked at the age and outcomes for all patients with stage T1-T3 who were treated with definitive radiotherapy, defined as a dose of 60 Gy or greater, and who hadn’t received hormonal therapy for any PSA recurrence. Patients who had received adjuvant or salvage radiotherapy after radical prostatectomy were excluded, as were patients with fewer than three follow-up PSA values.
Looking at age as both a continuous variable and comparing patients under 60 versus those 60 and older, the researchers found that age did not affect biochemical disease-free survival time.
"Other variables assessed for their predictive capability were pretreatment PSA level (p<0.001, significant), Gleason sum (p = 0.023, significant), stage (p = 0.828, not significant), and RT dose (p = 0.033, significant)," the authors wrote.
However, the data collected by the researchers didn’t address the "therapeutic adequacy" of radiotherapy (RT) versus radical prostatectomy (RP) in younger patients. "The differences between RP and RT populations in terms of patient performance status, nodal status, and clinical versus pathologic stage and grade are well documented," the authors wrote. "A contemporary bias is that younger patients should be offered RP, but little clinical evidence is available to support this bias."
The researchers also noted that their findings were in line with other more recent studies on the effect of age in prostate-cancer survival, in contrast with the older studies that suggested that younger patients were subject to more virulent disease. Therefore, the authors concluded, "physicians counseling patients regarding potential therapies should not be biased by patient age."
By Tracie L. ThompsonAuntMinnie.com contributing writer
March 24, 2003
Related Reading
Screening for colorectal cancer lags behind prostate cancer testing in U.S., March 19, 2003
Predictors of PSA relapse after radiotherapy for prostate cancer identified, May 17, 2003
Older age predicts shorter survival with high-risk prostate cancer, January 28, 2003
Studies illustrate benefits of FDG-PET, pre-planning in radiotherapy, January 27, 2003
Prognosis of high Gleason score, low PSA prostate cancer surprisingly good, January 7, 2003
Copyright © 2003 AuntMinnie.com