One discipline stays above the surface while the other hunts for what lies beneath, so it makes perfect sense that dermatology and radiology can complement one another. At the 2006 American Academy of Dermatology (AAD) meeting in San Francisco, imaging and skin specialists from the Mayo Clinic in Jacksonville, FL, and the Armed Forces Institute of Pathology in Washington, DC, offered advice on how to select the appropriate modality for evaluating cutaneous masses or defects.
"If a dermatologist considers radiologic imaging before biopsy, there can be difficulty deciding which type of study would be most appropriate," wrote the team, which included radiologist Dr. Mark Kransdorf from the Mayo Clinic, in a poster presentation.
The group covered which modality would be best for midline tumors, soft-tissue tumors, inflammatory signs of internal malignancy, infectious lesions, and metastatic lesions.
For evaluating midline lesions, the specialists recommended MRI. They described a case of a 59-year-old male with a birthmark on the back that caused some discomfort. A sagittal, T2-weighted MR of the upper thoracic spine showed some bifid T5 spinous process with abnormal configuration of the thecal sac. The spinal cord was normal.
"A fibrous connection between the thecal sac and the skin was present without any open communication between the thecal sac and the skin surface," the authors wrote. In this case, MR, with and without contrast, was performed for localization of the lesion. MR is best for central nervous system lesions in order to show nerve root or thecal sac entrapment, they added.
In another case that illustrated a soft-tissue tumor, a 45-year-old man presented with a new lesion on the left thigh. A physical exam could not determine the extent or depth of the lesion. An x-ray revealed a large medial mass on the left distal thigh. An unenhanced axial CT showed a large mass with superficial ulceration.
Imaging exams can offer more information as to whether a tissue is solid or cystic, the authors said. As an example, they described the case of a 7-year-old boy with a lesion on the left neck. An axial, contrast-enhanced CT demonstrated a calcified mass with delicate ossification. The CT scan aided in ruling out a cyst and helped the dermatologist come to a diagnosis of pilometricoma.
In a pediatric population, MR does offer minimum radiation exposure and is useful for localizing lesions, the authors stated, but the advantage of the CT scan is that sedation is not required.
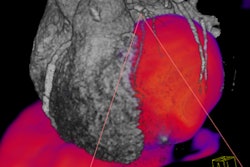
For metastatic lesions, the authors found MRI and PET imaging of value. They cited the case of a 68-year-old female with a history of melanoma who presented with a new mass on the right thigh. She underwent MR with a protocol of sagittal T1-weighted imaging, axial gadolinium-enhanced imaging, and fat suppressed T1-weighted imaging. The MR exam showed a well-defined, subcutaneous sold mass with intense homogeneous enhancement. Meanwhile, on the axial PET scan, two hypermetabolic foci were seen. They diagnosed her with melanoma metastases.
Finally, for inflammatory signs -- such as a smoker who presented with a rash -- chest x-ray can reveal perihilar masses while CT can delineate soft-tissue masses. And to illustrate how imaging works for infectious lesions, the authors described a diabetic with an ulceration on the heel. And indium-111 scan showed osteomyelitis. A nuclear medicine test was performed because the patient, who had a pacemaker, was ineligible for MRI. In addition, a CT scan would not have detected edema.
By selecting the right imaging modality, dermatologists can determine the extent, anatomic location, and tissue type of various lesions, the authors stated.
By Shalmali Pal
AuntMinnie.com staff writer
April 6, 2006
Related Reading
PET/CT imaging useful in detecting and staging choroidal melanomas, November 8, 2005
Wide excision can avoid need for radiation with desmoplastic melanoma, October 7, 2005
Copyright © 2006 AuntMinnie.com